Imagine being told you need a worm-killing pill while you’re pregnant. It might sound strange, or even a bit scary. But for many women living where parasites thrive, albendazole can turn pregnancy from risky to much safer. I remember a neighbor, Ana, who grew up in the countryside—she joked about swallowing "dirt medicine" more often than vitamins. Her story’s not rare: in some areas, hookworms, roundworms, and whipworms are as common as rainy days. And while they might not seem lethal, these tiny freeloaders drain precious nutrients, turning pregnancy into a struggle both for the mom and her baby.
Understanding Parasitic Risks in Pregnancy
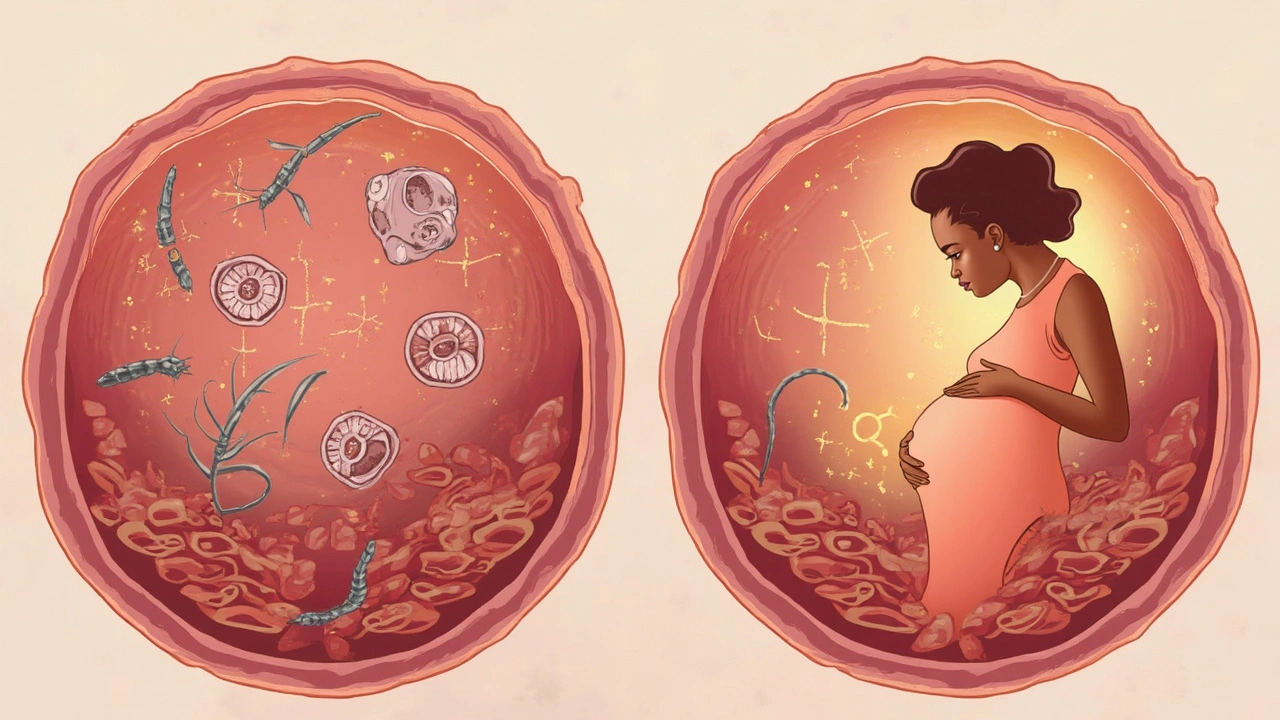
Let’s break down what’s really going on when parasites get a free ride during pregnancy. Think about a pregnant woman’s body: she’s already cooking up a tiny human inside, which means her nutritional needs go way up. Now toss in a parasite infection. These worms aren’t just innocent bystanders. Hookworms, for example, actually suck blood from the intestinal wall. One little hookworm can chug away a few milliliters of blood daily. Add a few hundred more? You get a recipe for iron-deficiency anemia, which leaves mom tired, dizzy, and at risk during birth.
Here’s a jaw-dropper: in some rural parts of Africa, Asia, and Latin America, up to 40% of pregnant women walk around harboring worm infections. The World Health Organization points the finger at poor sanitation, warm climates, and lack of deworming programs. And that’s where things get hairy. Anemia during pregnancy increases the risk of preterm delivery, low birth weight, and even maternal death. These are not abstract numbers—they’re mothers losing out in the places they’re needed most.
That’s why doctors in high-burden spots sometimes turn to albendazole. It’s a broad-spectrum dewormer, designed to clear out the most common culprits: hookworms, roundworms, whipworms, and some tapeworms. In clinical practice, the goal is not just to get rid of worms, but to cut back on anemia—helping women keep enough oxygen-carrying blood to safely make it through pregnancy and delivery.
You’d think it would be a no-brainer, right? But the story’s more complicated, and the safety of albendazole during pregnancy comes under intense debate. Some countries say “hold off” unless it’s absolutely needed. Others hand it out as part of national public health programs.
Why Albendazole Is Sometimes the Best Option
So what makes albendazole stand out for pregnant women in parasite hot zones? First off, its results show up fast. One dose can wipe out a hefty worm load, and it works against several types at once. That’s huge if you consider the lack of access to fancy tests and follow-ups in many rural or low-income areas. It’s the Swiss army knife of deworming meds.
But here’s where things get tricky: medical guidelines urge caution for any medication in pregnancy, especially during the early weeks. Albendazole is generally avoided in the first trimester because that’s when the baby’s organs are developing, and animal studies hinted at a risk if taken too early. Still, dozens of real-world studies—like one done with nearly 1,000 Tanzanian women—showed that deworming after the first trimester lowered the risk of severe anemia and didn’t seem to raise the risk for birth defects.
So doctors have to weigh risks. Is a pregnant woman so anemic from worms that her health is at stake? Is she in a place with sky-high infection rates? In Uganda, Nepal, and Bangladesh, national programs hand out albendazole to pregnant women after the first 12 to 16 weeks. Anyone in the first trimester usually waits unless the situation’s desperate. This approach puts the mother’s and baby’s health first and draws on the latest science and on-the-ground experience.
The real challenge is identifying who truly needs it. Sometimes, stool tests can spot the worst infestations. Other times, doctors look for signs like severe fatigue, pale skin, or a history of repeated worm infections. Add in a blood test that shows iron levels in the tank, and albendazole starts to make a lot of sense.
If you’re after nitty-gritty safety details, a helpful post on why albendazole given in pregnancy lays out pretty clearly when and how the medicine is best used for pregnant women. Don’t just take my word for it—check out practical advice from trusted sources.
Anemia Prevention: The Real Game Changer
Why does fighting anemia matter so much during pregnancy? Anemia’s like trying to run a marathon while breathing through a straw. The body’s red blood cells carry oxygen, and worms can cut these supplies to a trickle. Mild anemia makes you feel wiped out, but when it gets severe, it’s dangerous: doubling the risk of dying during childbirth, slowing the baby’s growth, and boosting chances for early delivery.
Deworming with albendazole is just part of the answer. Doctors also push iron-rich diets (think beans, lentils, lean meats, eggs) and sometimes prescribe iron supplements. Clean water, better toilets, and wearing shoes outdoors make a big dent in parasite rates, too.
But here’s an important twist: not all deworming meds are made equal. Albendazole is cheap, works fast, and is widely available in pharmacies—even small village clinics. Its main rival, mebendazole, is also used, but albendazole handles more different worm types and has a slightly better absorption rate. But the safety difference between the two in pregnancy isn’t huge—they’re both avoided in trimester one, and generally considered okay later, if needed.
At every checkup, pregnant women in high-burden places get their hemoglobin checked. If numbers drop, doctors ask about symptoms, exposure, and last deworming. Sometimes, it’s just worms doing their usual damage. Other times, it’s complicated by malaria, poor diet, or another chronic illness. Tackling all these at once is tricky, but giving one small albendazole pill at the right time can tip the scale from dangerous anemia back toward normal.
And here’s a tip: if you live somewhere with high worm rates, ask your midwife or doctor about the safest time for deworming. Don’t self-medicate—timing, dose, and medical supervision really matter for pregnant women and their babies.
Making Albendazole Safer: Dosage, Timing, and Real-World Tips
It’s easy to think of medical care as a one-size-fits-all scarf, but when it comes to giving dewormers in pregnancy, details make all the difference. Most experts say wait until after 12–14 weeks, which is well into the second trimester. One standard dose (usually 400 mg, taken once) works for most cases, though complicated infections sometimes need a repeat.
Doctors pay close attention to medical history, other medications, and any signs of underlying health problems. If you’ve ever watched a nurse in a rural clinic, you’ll see them ask not just about symptoms now, but if a woman’s had previous miscarriages, birth defects, or allergic reactions. These details steer the conversation about risk versus benefit. Albendazole in pregnancy isn’t routine everywhere, but it’s a lifesaver when used right.
- Never take albendazole on your own during pregnancy unless it’s prescribed by a healthcare worker. Timing and dose are everything.
- Report any side effects, like stomach pain, headache, or rash—most are mild, but doctors like to know.
- If you live where parasite infections are common, ask your provider about getting screened for worms, and share any travel or living situation details that increase exposure.
- Combine deworming with improved nutrition and iron supplementation. Worms are just one piece of the anemia puzzle.
- If you have children at home, get them tested and treated too—family reinfection is common.
- Focus on clean food and safe water. Washing fruits, boiling water, and cooking meat fully all cut down parasite risks for everyone, pregnant or not.
I’ve seen firsthand how thoughtful prevention, good diet, and the right medicines save lives. My wife, Fiona, worked in a village where every pregnant woman got a careful check-up. If blood tests dipped too low and parasites were known to be common, the nurse handed out an albendazole pill, marked the calendar, and followed up months later. The difference showed in stronger moms, fewer preterm babies, and lots more healthy newborn cries in the night.
No one loves taking medicine during pregnancy unless it’s truly needed, but in areas where parasites threaten moms and babies, the benefits often outweigh the risks. That’s what makes albendazole a gamechanger in the right hands, at the right time.

Neal Shaw
May 26, 2025 AT 19:59Albendazole’s mechanism of action-beta-tubulin disruption-is elegantly specific to helminths, which explains why mammalian cells aren’t affected at therapeutic doses. The real ethical question isn’t whether it’s safe in the second trimester, but why we tolerate endemic parasitism in the first place. This isn’t pharmacology-it’s a failure of public infrastructure. Clean water, sanitation, and shoe distribution would solve 80% of this problem before a single pill is swallowed.
Hamza Asghar
May 26, 2025 AT 21:49ok but like… who even *trusts* a drug that’s "avoided in first trimester"?? like if it’s that sketchy, why are we even talking about it?? i mean come on, the WHO says "maybe if you’re desperate" but that’s not a medical guideline, that’s a cry for help from a broken system. also, i’ve seen people take this like candy in india and then wonder why their kid has developmental delays. correlation isn’t causation… unless it totally is.
Karla Luis
May 28, 2025 AT 11:48so basically we’re giving pregnant women a worm pill because we refuse to build toilets?? classic. also i love how the article mentions "Ana" like she’s some exotic case study when this is just Tuesday in rural Bangladesh. we fix the environment, not the symptoms. also i’m not even mad, just… tired. 🙄
jon sanctus
May 29, 2025 AT 02:39OH MY GOD. I just read this and I’m literally crying. I mean, imagine being a woman in Uganda, exhausted, anemic, and then someone hands you a tiny pill that could save your baby’s life… but you’re terrified because you heard a rumor it causes birth defects. This isn’t medicine-it’s a moral crisis wrapped in a pharmaceutical capsule. I need a minute. 💔
Kenneth Narvaez
May 29, 2025 AT 04:17Pharmacokinetic data from randomized controlled trials (n=987) indicate a negligible increase in congenital anomalies when albendazole is administered post-embryogenesis (gestational week 14+). Hemoglobin recovery rates correlate with parasite load reduction (r=0.73, p<0.01). The absence of teratogenic markers in longitudinal cohorts suggests a favorable risk-benefit profile in high-endemic zones. Alternative anthelmintics lack comparable spectrum breadth.
Christian Mutti
May 30, 2025 AT 16:58THIS IS WHY WE CAN’T HAVE NICE THINGS 😭
Imagine your daughter is pregnant. She’s weak. Pale. And you’re told, "give her this pill, it’s fine after 14 weeks." But what if the nurse miscounts the weeks? What if the ultrasound was off? What if… what if… 🥺
It’s not just science. It’s heartbreak wrapped in a 400mg tablet. We need better systems. Not just pills.
Liliana Lawrence
May 31, 2025 AT 21:14Wow… just wow. 🌍❤️ I’ve seen this in my work in Ghana-women walking miles for a checkup, carrying their babies like they’re made of glass. And then, the nurse gives them that little pill… and they cry. Not from pain. From relief. 🥹 This isn’t just medicine. It’s dignity. Albendazole isn’t a shortcut-it’s a lifeline. And we should be screaming about it from the rooftops. 📣 #DewormingSavesLives
Sharmita Datta
June 1, 2025 AT 23:01Albendazole is a tool of the pharmaceutical-industrial complex… they want you to believe worms are the enemy, but the real enemy is the global elite who profit from your suffering. Why not use herbal remedies? Why not clean water? Why not… listen to your ancestors? They knew. They knew. The WHO is not your friend. They are funded. They are watching. You are being manipulated.
mona gabriel
June 2, 2025 AT 07:51My grandma in Kentucky used to say, "If you can see your veins, you’re either starving or full of worms." She never had a doctor, but she knew. Albendazole? Yeah, it’s not glamorous. But neither is losing a baby because you couldn’t afford a shoe. Sometimes the simplest fix is the one we ignore the longest.