Chest Congestion Assessment Tool
Assess Your Symptoms
Answer these questions to determine if you should seek medical attention.
When you feel chest congestion is a build‑up of mucus and fluid in the lungs and airways that makes breathing feel heavy or rattly, you know something isn’t quite right. It might be a lingering cold, an allergic flare‑up, or simply irritation from dry air. Understanding what’s actually happening inside your chest helps you decide whether a glass of water, a humidifier, or a doctor’s visit is the right move.
Key Takeaways
- Chest congestion is caused by excess mucus, inflammation, and narrowed airways.
- Viruses, bacteria, allergies, and reflux are the most common triggers.
- The body’s cough reflex and cilia work together to clear the blockage.
- Home care works for mild cases; warning signs include fever > 38°C, shortness of breath, or blood‑streaked sputum.
- Staying hydrated, using steam, and avoiding irritants speed recovery.
What Exactly Is Chest Congestion?
At its core, chest congestion refers to the accumulation of mucus, fluid, or cellular debris in the lower respiratory tract. This buildup interferes with normal airflow, creating that familiar “tight” or “wet” feeling in the chest. While the term is often used interchangeably with “phlegm” or “cough,” it actually describes the whole environment inside the lungs and bronchial passages during an episode of excess secretions.
The Physiology Behind the Mucus Build‑Up
The respiratory tract is a network of airways that starts at the nostrils and ends in the alveoli where gas exchange occurs is lined with goblet cells that constantly produce mucus a sticky, water‑based fluid that traps dust, microbes, and other particles. Under normal conditions, tiny hair‑like structures called cilia beat in synchronized waves, pushing the mucus upward toward the throat where it’s either swallowed or expelled as a cough.
When an irritant or infection shows up, the body ramps up mucus production to trap the invader more effectively. At the same time, the bronchial tubes the main passages that carry air into the lungs swell-a process called inflammation the immune system’s response that increases blood flow and fluid leakage into tissue. Swelling narrows the airway lumen, so even a modest amount of mucus can feel obstructive.
The cough reflex a protective mechanism that forces a sudden expulsion of air to clear the airways kicks in when receptors in the airway walls sense irritation. A productive cough tries to dislodge the thickened secretions, while a dry cough often signals that the mucus is still too viscous to move.
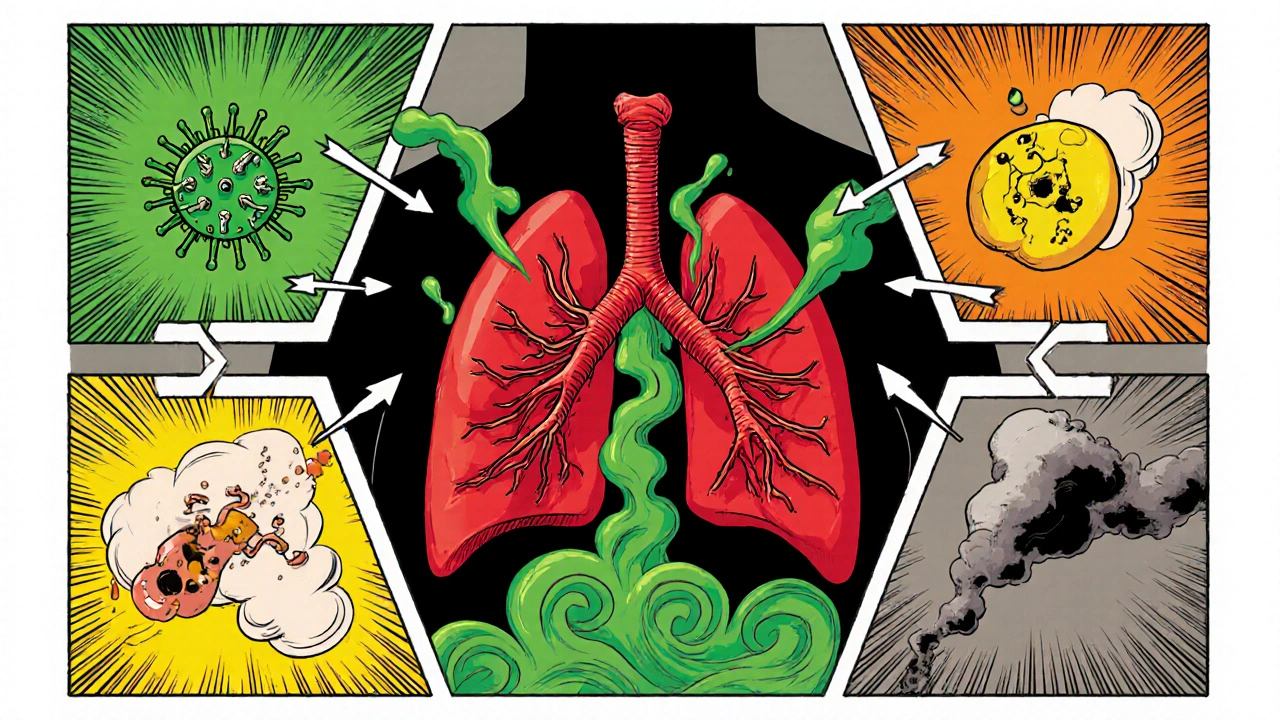
What Triggers Chest Congestion?
Many factors can set off the cascade described above. Below is a quick comparison of the most common culprits, their typical onset, and what to watch for.
| Cause | Typical Onset | Main Symptoms | When It Usually Resolves |
|---|---|---|---|
| Upper respiratory infection (cold) | 1‑3 days after sore throat | Runny nose, mild fever, productive cough | 7‑10 days |
| Bacterial bronchitis | After a viral cold, worsening after 5 days | Fever >38°C, colored sputum, fatigue | 10‑14 days with antibiotics |
| Allergies | Seasonal or exposure to triggers | Itchy eyes, clear mucus, wheezing | As long as allergen exposure continues |
| Asthma flare‑up | Cold air, exercise, stress | Chest tightness, whistling breath, cough | Variable; controlled with inhalers |
| Gastro‑esophageal reflux (GERD) | After meals, lying down | Burning throat, sour taste, cough at night | Improves with diet and meds |
Notice how viral infections often start with a sore throat and progress to a productive cough, whereas allergies usually bring clear, watery mucus and itchy eyes. Recognising the pattern helps you pick the right coping strategy.
How Your Body Signals Trouble
Beyond the obvious cough, a few other signs tell you the lungs are fighting back. A rattling sound-called rhonchi-occurs when air passes over thick secretions. Tightness across the chest can mean the bronchial tubes are inflamed. If you notice a fever higher than 38°C (100.4°F) or feel unusually short of breath, the inflammation may be more than a simple viral cold.
The color of sputum also offers clues. Clear or white mucus is typical for viral infections and allergies. Yellow or green sputum suggests a bacterial component, as immune cells release enzymes that tint the fluid. Blood‑streaked sputum isn’t common and should prompt a medical review immediately.
When to Seek Professional Help
Most chest congestion clears on its own with rest and hydration, but there are red flags that merit a doctor’s visit:
- Fever persisting beyond three days or spiking above 39°C (102.2°F).
- Shortness of breath at rest or worsening exertional dyspnea.
- Chest pain that feels sharp, especially when breathing deeply.
- Sputum that’s dark, thick, or contains blood.
- Symptoms lasting longer than two weeks without improvement.
If any of these appear, a healthcare professional may order a chest X‑ray, sputum culture, or spirometry test to pinpoint infection or underlying chronic disease.
Home Care Strategies That Really Work
For mild to moderate cases, simple measures can speed recovery:
- Stay hydrated. Water, herbal teas, and clear broths thin mucus, making it easier to cough up.
- Use a humidifier or take a hot shower to add moisture to the air; the steam loosens sticky secretions.
- Try an over‑the‑counter expectorant containing guaifenesin; it helps the cilia move mucus upward.
- Elevate your head while sleeping to reduce post‑nasal drip and reflux‑related irritation.
- Avoid smoking, second‑hand smoke, and strong fragrances that further inflame the airways.
For allergy‑driven congestion, antihistamines or nasal corticosteroid sprays can curb mucus production. If GERD is the culprit, meals should be finished two hours before bedtime, and a proton‑pump inhibitor may be prescribed.
Frequently Asked Questions
Why does chest congestion feel worse at night?
When you lie down, gravity no longer helps drain mucus from the upper airways. In addition, cooler nighttime air can narrow bronchi, making the sensation of blockage more noticeable.
Can I exercise while I have chest congestion?
Light activity like walking is fine if you can talk without coughing. Intense cardio may worsen inflammation and trigger a stronger cough, so it’s best to hold off until you feel breathless‑free.
Is it safe to use a hot water bottle on my chest?
A warm compress can ease muscle tightness, but it won’t clear mucus. Use it for comfort only and avoid excessive heat that could burn the skin.
Do antibiotics help with chest congestion?
Only if a bacterial infection is confirmed. Most colds and viral bronchitis resolve without antibiotics; unnecessary use can lead to resistance.
How long should I expect chest congestion to last?
Typical viral congestion eases in 7‑10 days. If symptoms linger beyond two weeks, or you develop new red‑flag signs, seek medical evaluation.
Understanding the chain of events-from mucus production to coughing-gives you the power to choose the right remedy and know when professional help is needed. Keep hydrated, watch for warning signs, and treat the root cause, not just the symptom.

Welcher Saltsman
October 15, 2025 AT 18:30Stay hydrated and you'll be breathing easier soon
april wang
October 15, 2025 AT 19:04Chest congestion can feel like a stubborn fog inside your lungs, but it’s really just your body trying to flush out invaders.
The first thing I always recommend is to keep the fluids coming, because water thins the mucus and makes the cough more productive.
Even a warm herbal tea with honey can soothe the throat while the steam works on loosening the sticky secretions.
If you have a humidifier, set it to a comfortable level and let the moisture drift through the room; it’s like giving your airways a gentle massage.
Over‑the‑counter expectorants such as guaifenesin are designed to shake up the mucus so the cilia can push it upward more efficiently.
For allergy‑related bouts, an antihistamine or a nasal steroid spray can cut down the extra mucus production at the source.
When reflux is the culprit, elevating the head of the bed and avoiding heavy meals before bedtime can make a huge difference.
It’s easy to overlook the impact of irritants like cigarette smoke or strong fragrances, so keeping your environment clean helps the healing process.
Listening to your body’s warning signs is crucial – a fever above 38 °C, shortness of breath, or blood‑streaked sputum are red flags that deserve a doctor’s look.
Most viral infections will run their course in about a week, but if symptoms linger beyond two weeks you should get checked out.
Simple breathing exercises, like slow diaphragmatic breaths, can improve airflow and give you a sense of control over the tightness.
If you’re an asthmatic, make sure your rescue inhaler is handy and follow your action plan; sometimes a flare‑up can masquerade as congestion.
Staying upright while you’re drinking fluids or taking medication can help gravity do its part in draining the mucus.
A hot shower not only adds steam but also relaxes the chest muscles, which can reduce that uncomfortable feeling of pressure.
Remember that antibiotics only work on bacterial infections, so using them for a plain cold won’t speed up recovery and can contribute to resistance.
In short, hydrate, humidify, and heed any warning signs, and you’ll give your lungs the best chance to clear out the congestion on their own.
Vishnu Raghunath
October 15, 2025 AT 19:37Oh yeah, because drinking tea is going to chase away a virus, right? It's like expecting a magic wand to fix everything.
Aparna Dheep
October 15, 2025 AT 20:10One must consider that the very notion of congestion is but a philosophical metaphor for the human condition's resistance to change.
We speak of clearing the lungs as if we could simply sweep away existential dread with a cough.
Edward Glasscote
October 15, 2025 AT 20:44I noticed that when I sleep with an extra pillow, the nighttime cough eases up a bit.
Gaurav Joshi
October 15, 2025 AT 21:17All that steam talk sounds like hype; I just open a window and let the fresh air do its job.
Jennifer Castaneda
October 15, 2025 AT 21:50Sure, the “tea cure” is just the tip of a larger agenda to keep us dependent on commercial health hacks.
They want us to believe that a soothing sip will mask the deeper inflammation that only a thorough medical check can reveal.
Annie Eun
October 15, 2025 AT 22:24The night feels endless when your chest is clogged; I keep asking why my body decides to betray me at the worst moments.
Jay Kay
October 15, 2025 AT 22:57Guaifenesin works by thinning mucus so you can cough it out
Franco WR
October 15, 2025 AT 23:30I totally get that, the way it loosens the mucus feels like giving the lungs a gentle push.
When you combine it with plenty of fluids, the effect is almost noticeable within a few hours.
Plus, staying upright and breathing slowly helps the expectorant do its job more efficiently.
Just remember to follow the dosage and not overdo it, otherwise you might end up with a runny nose instead.
😊 Stay consistent and you should feel the difference soon.
Rachelle Dodge
October 16, 2025 AT 00:04Mucus is nature's reminder that even our bodies need to pause and cleanse.
Gaurav Joshi
October 16, 2025 AT 00:37Indeed, the act of coughing is a tiny rebellion against stagnation, a purposeful expulsion of what no longer serves.
Elaine Proffitt
October 16, 2025 AT 01:10Good summary of when to see a doctor.
Christopher Munt
October 16, 2025 AT 01:44👍 Stay patient, your lungs will thank you!
Mike Creighton
October 16, 2025 AT 02:17Each breath amidst congestion is a silent proclamation that life persists, fighting against the veil of opacity that seeks to silence us.
Desiree Young
October 16, 2025 AT 02:50i cant stress enough that you need to stop ignoring the red flags they are real and dont go away
Vivek Koul
October 16, 2025 AT 03:24In summary, appropriate self‑care measures complemented by timely medical evaluation constitute a comprehensive approach to managing chest congestion.