Why You Should Never Leave the Pharmacy Without Confirming Your Medication
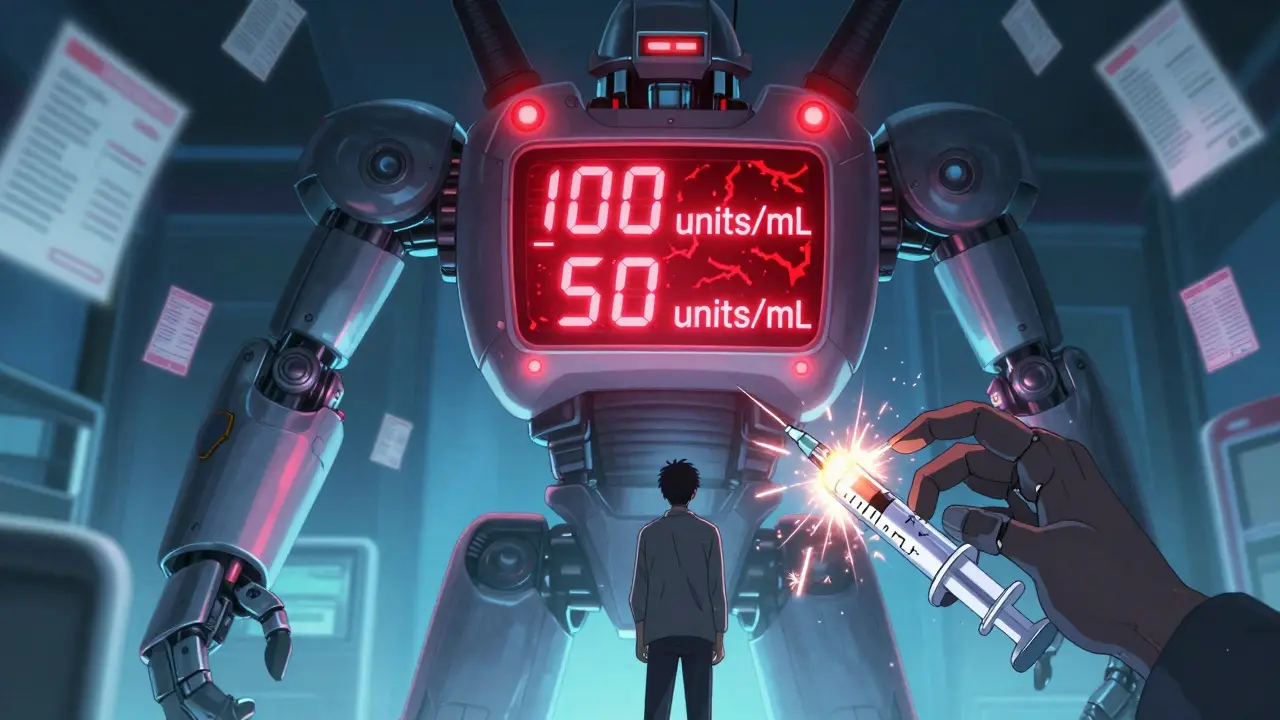
Imagine this: you pick up your prescription for insulin, the pharmacist hands you the bottle, you nod, pay, and walk out. Two days later, you inject what you think is your usual dose-and end up in the emergency room. The bottle had 100 units per mL, but the label said 50. You took twice as much as you should have. This isn’t a hypothetical. It’s happened. And it’s preventable.
The truth is, mistakes happen in pharmacies. Not because pharmacists are careless, but because the system is complex. Prescriptions get misread. Labels get printed wrong. Doses get miscalculated. And if no one stops to double-check, the error reaches you.
That’s why double-checking medication strength and quantity before you leave the pharmacy isn’t just good practice-it’s your last line of defense.
What Exactly Is a Medication Strength Error?
Strength errors sound technical, but they’re simple to understand. They happen when the amount of active drug in a dose is wrong. For example:
- You’re prescribed 5 mg of lisinopril, but you get 10 mg.
- You’re given liquid amoxicillin labeled as 250 mg per 5 mL, but it’s actually 500 mg per 5 mL.
- You think you’re getting 1 mL of insulin, but the syringe holds 10 mL because the label confused concentration with total volume.
These aren’t small mistakes. The FDA reports that over 60% of fatal medication errors involve high-alert drugs like insulin, opioids, and blood thinners-and strength errors are the #1 cause. A 2023 study from the Institute for Safe Medication Practices found that 87% of these errors could have been caught if someone had verified the total amount of drug in the container before dispensing.
How Pharmacists Are Supposed to Catch These Errors
Accredited pharmacies in the U.S. follow strict guidelines set by the ISMP, USP, and The Joint Commission. Here’s what a proper double-check looks like:
- Verify the strength-Look at the label and confirm the amount of drug per unit (e.g., 5 mg per tablet, 100 units per mL). This isn’t just reading the label-it’s mentally comparing it to the prescription.
- Count the quantity-If you’re prescribed 30 pills, are there exactly 30? If it’s liquid, is the bottle volume correct? A 100 mL bottle shouldn’t be labeled as 50 mL.
- Recalculate independently-If the prescription says 2.5 mL twice daily, and the concentration is 5 mg/mL, the total daily dose should be 25 mg. Does that match the doctor’s order? A second person should do this math separately.
- Check the dosing device-Was an oral syringe provided for liquids? Or just a teaspoon? Household spoons vary in size and cause 93% of pediatric dosing errors, according to ISMP data.
- Confirm labeling standards-The strength should be the largest, most prominent text on the label. Concentration (e.g., “per mL”) should be smaller. If the label says “50 mg/mL” in big letters but doesn’t clearly say “Total: 100 mg,” it’s a red flag.
Pharmacies using barcode scanning and electronic verification cut dispensing errors by 83%, but even then, human review is still required. Technology helps-but it doesn’t replace the need for a second set of eyes.

What You Can Do to Protect Yourself
You don’t have to rely on the pharmacist alone. You can-and should-be part of the safety net.
- Ask: “Is this the right dose?” Don’t say “Does this look right?” Say: “I was prescribed 5 mg, and this bottle says 10 mg per tablet. Is that correct?” Specific questions force a real check.
- Compare the label to your prescription-If you have a printed copy or a photo of your prescription, hold it up to the label. Match the drug name, strength, quantity, and directions.
- Check the dosing tool-If you’re getting liquid medicine, ask for an oral syringe. Never use a kitchen spoon. Even “teaspoon” on the label doesn’t mean it’s accurate.
- Watch for decimals-A dose of 0.5 mL is not the same as 5 mL. Always look for leading zeros (0.5, not .5) and never trust trailing zeros (5.0 mL is dangerous-it can be misread as 50 mL).
- Speak up if something feels off-If the pill looks different, the bottle size seems wrong, or the instructions confuse you, pause. Ask again. Walk out and call the pharmacy back if needed.
One pharmacist in Sydney told me about a patient who came back a week later saying, “I didn’t think to check, but I realized I was taking twice the dose.” She was on warfarin. A 10-fold error could have caused internal bleeding. She survived because she noticed the pattern. Don’t wait for symptoms. Check before you leave.
Why This Isn’t Just a “Pharmacist’s Job”
Many people think, “The pharmacist is trained. They’ll catch it.” But staffing is tight. In community pharmacies, technicians are often expected to process 35+ prescriptions per hour. That’s less than two minutes per script. There’s no time for deep checks.
Studies show that pharmacies with structured double-check protocols have 78% fewer strength-related errors. But only 43% of community pharmacies consistently follow all steps. Independent pharmacies with fewer staff are especially vulnerable. One Reddit user shared how a coworker skipped the check during a busy shift and accidentally dispensed 10 times the dose of levothyroxine. The patient was hospitalized.
This isn’t about blame. It’s about shared responsibility. Your life is on the line. If you don’t verify, no one else will.
What’s Changing to Make This Safer
There’s progress. In 2023, the FDA issued draft guidelines requiring all injectable medications to display the total drug amount in bold, oversized text by 2025. USP is pushing for digital verification systems that cross-check prescriptions against national drug databases. Medicare Part D now requires pharmacies to prove they have strength verification protocols to stay in network.
But change is slow. Labels still get printed wrong. Staff still get rushed. And patients still leave without asking questions.
The best safety system isn’t a new app or a barcode scanner. It’s a patient who knows enough to ask: “Is this right?”

Real Consequences, Real Stories
A 2022 case in Melbourne involved a child given 5 mL of acetaminophen instead of 0.5 mL because the pharmacy handed out a teaspoon. The child developed liver failure. The label said “160 mg/5 mL,” but the parent assumed the entire bottle was for one dose. The pharmacy had provided no oral syringe. No counseling. No double-check.
Another case: an elderly man on warfarin was given 5 mg tablets instead of 1 mg. He didn’t notice the difference. Two weeks later, he had a stroke from excessive thinning of his blood.
These aren’t rare. The Joint Commission found that 68% of all serious medication events from 2020 to 2022 involved inadequate strength verification. Most of them happened at the pharmacy counter.
Final Reminder: Don’t Just Take It-Verify It
You wouldn’t drive a car without checking the brakes. You wouldn’t plug in a device without checking the voltage. Why would you take a medicine without checking the dose?
It takes 30 seconds. Two questions: “Is this the right strength?” and “Is this the right amount?”
That’s all it takes to prevent a hospital visit, a life-altering injury, or worse.
Next time you pick up a prescription, pause. Look. Ask. Confirm. Then walk out-knowing you did everything you could to stay safe.
What should I check on my medication label before leaving the pharmacy?
Look for the drug name, strength (e.g., 10 mg per tablet), total quantity (e.g., 30 tablets), and the concentration if it’s liquid (e.g., 5 mg/mL). The strength should be the largest text on the label. Make sure the total amount in the container matches what was prescribed. If it’s liquid, confirm an oral syringe was provided-not a kitchen spoon.
Can I trust the pharmacist to catch all mistakes?
Most pharmacists try their best, but they’re often under time pressure. In many community pharmacies, staff are expected to process over 35 prescriptions per hour. That leaves little room for deep verification. Studies show that errors drop by 78% when double-checking is mandatory. Don’t assume it’s happening. Ask questions yourself.
Why is using a teaspoon dangerous for liquid medicine?
Household teaspoons vary in size-from 3 mL to 7 mL. Medical dosing requires precision. A teaspoon might deliver 2-3 times more than the prescribed dose. The ISMP reports that 93% of pediatric liquid medication errors involve spoon confusion. Always use the oral syringe or dosing cup provided by the pharmacy.
What’s the difference between strength and total quantity?
Strength is how much drug is in each unit-for example, 5 mg per tablet. Total quantity is how many units you’re getting-like 30 tablets. If you’re prescribed 5 mg twice daily for 14 days, you should get 28 tablets. If you get 100, that’s a 3.5-fold overdose. Always confirm both numbers.
Are some medications more dangerous if the strength is wrong?
Yes. High-alert medications like insulin, opioids, blood thinners (warfarin), and thyroid drugs can cause death or serious harm with small errors. For example, giving 10 units of insulin instead of 1 can cause a life-threatening low blood sugar. Always double-check these especially.
What should I do if I realize I got the wrong dose after leaving the pharmacy?
Call the pharmacy immediately. Do not take any more of the medication. If you’ve already taken it and feel unwell, go to the nearest emergency room or call emergency services. Keep the bottle and packaging-they’ll help medical staff understand what happened.
What to Do Next
Make this a habit. Before you leave the pharmacy, do this:
- Hold the bottle and label in one hand.
- Open your phone or wallet and pull out your prescription or a photo of it.
- Compare the drug name, strength, and total quantity.
- Check the dosing device-did you get a syringe?
- Ask one clear question: “Is this exactly what was prescribed?”
That’s it. Five seconds of your time. It could save your life-or someone else’s.