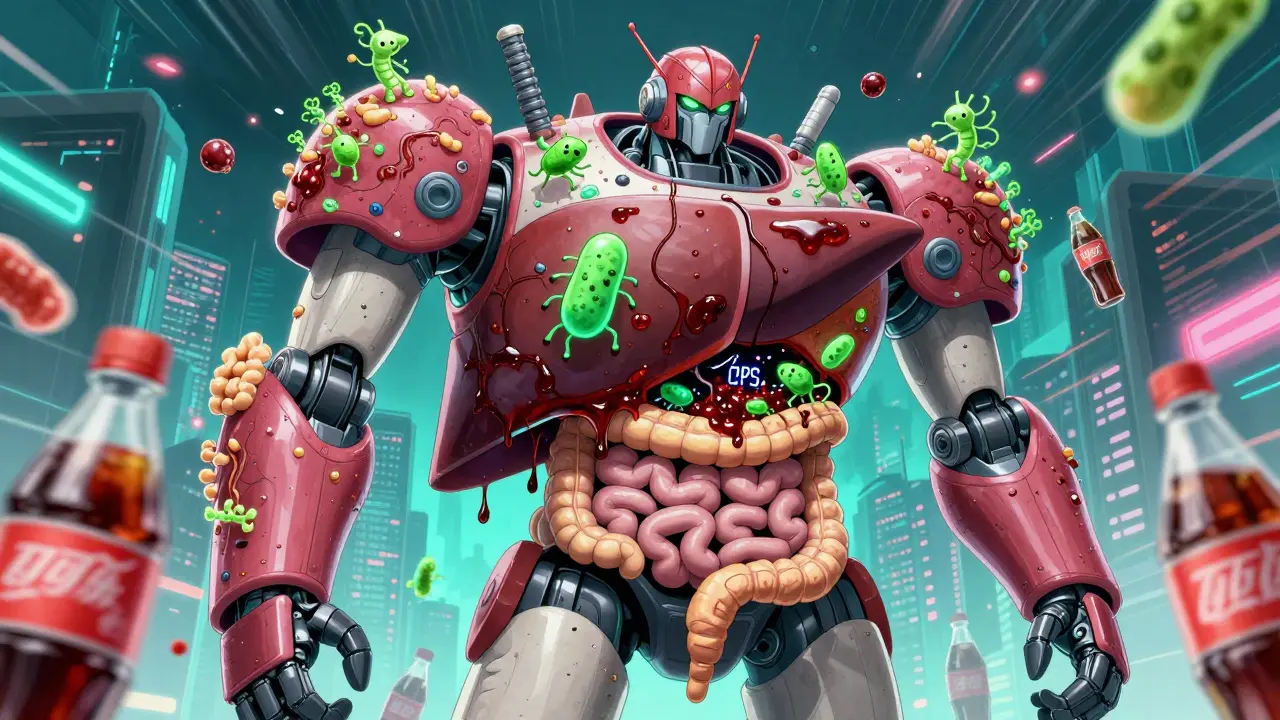
When your liver gets fatty-not from drinking alcohol, but from too much sugar, refined carbs, and sitting around-it’s not just a weight issue. It’s a gut issue. Nonalcoholic fatty liver disease (NAFLD), now more accurately called metabolic dysfunction-associated steatotic liver disease (MASLD), affects about one in three people worldwide. And the root cause isn’t just eating too much-it’s how your gut is talking to your liver, and whether it’s saying the right things.
The Gut-Liver Connection You Can’t Ignore
Your liver and your gut are connected by a highway called the portal vein. Every time you eat, nutrients, toxins, and bacteria from your intestines flow straight to your liver. Normally, your gut lining keeps bad stuff out. But in NAFLD, that lining gets leaky. Studies show about 90% of people with fatty liver have a damaged gut barrier. That means endotoxins like LPS-harmful bacterial byproducts-get into the bloodstream and trigger inflammation in the liver. In people with NAFLD, LPS levels are more than twice as high as in healthy people. This isn’t just about inflammation. Your gut bacteria also control bile acids, which help break down fat. When the wrong bacteria take over, they turn primary bile acids into secondary ones that mess with your liver’s fat-burning signals. At the same time, your good bacteria-like those that make butyrate-are disappearing. People with NAFLD have 58% less butyrate in their stool than healthy people. Butyrate is the fuel your gut lining needs to stay strong. No butyrate? Leaky gut gets worse. And the cycle keeps spinning.Diet Is the Most Powerful Tool You Have
Weight loss is the only proven way to reverse fatty liver. But not just any weight loss. Losing 5% of your body weight improves liver fat in 81% of people. Lose 10%, and nearly half of those with the more serious form (NASH) see their liver inflammation disappear. The key? How you lose it. The Mediterranean diet isn’t just trendy-it’s backed by hard data. A 6-month study with 70 NAFLD patients showed a 32% drop in liver fat when they ate more olive oil, vegetables, nuts, and whole grains, and cut back on sugar and processed food. Adding 30 grams of walnuts a day (about 10 halves) boosted the effect. Why? Walnuts are packed with fiber and polyphenols that feed good gut bacteria. They’re not just food-they’re prebiotics. Here’s what works:- Get 25-30 grams of fiber daily-from beans, oats, broccoli, apples, and chia seeds. Fiber feeds your good bacteria and reduces liver fat.
- Replace saturated fats with monounsaturated fats-olive oil, avocados, almonds. These reduce inflammation and improve insulin sensitivity.
- Avoid fructose-especially high-fructose corn syrup. More than 25 grams a day (think: soda, candy, flavored yogurts) directly fuels liver fat buildup.
- Don’t skip meals-eating too few calories too fast can backfire. Aim for a 500-750 calorie deficit per day. That’s 0.5-1 kg of weight loss per week. Slow and steady keeps the weight off and your liver healing.
Probiotics and Prebiotics: Helpful, But Not Magic
Probiotics won’t fix your liver alone. But when paired with diet and weight loss, they help. A 24-week study with 100 NAFLD patients showed that taking a daily mix of Lactobacillus rhamnosus GG, Bifidobacterium longum, and Streptococcus thermophilus cut liver fat by 23% and lowered liver enzymes by 31%. That’s as good as some medications-without the side effects. Prebiotics are even simpler. Just 10 grams of inulin (found in chicory root, onions, garlic) or 8 grams of fructo-oligosaccharides (FOS) daily for 12 weeks boosted butyrate by 47% and lowered liver stiffness by 15%. You can get these from food or supplements. No need to spend $60 a month on fancy bottles-plain inulin powder works fine. But here’s the catch: Not all probiotics are equal. The strains matter. Stick to ones with research backing: Lactobacillus reuteri NCIMB 30242 for bile acid control, or multi-strain blends with at least 10 billion CFUs daily. And give it time-12 weeks minimum. If you don’t see changes in digestion, bloating, or energy after that, try a different strain.
Why Weight Loss Alone Isn’t Enough
You might lose weight and think you’re done. But if your gut stays broken, the fat comes back. A Mayo Clinic study found that people who lost weight with a structured program-diet, exercise, and behavioral support-kept it off in 68% of cases after two years. Those who tried on their own? Only 29% kept the weight off. Why? Because NAFLD isn’t just about calories. It’s about insulin resistance, inflammation, and gut bacteria. Losing weight helps, but if you go back to eating processed food and sugar, your gut flips back to its old, harmful state. That’s why diet changes must stick. The best approach? Combine weight loss with gut-friendly eating. Don’t just count calories-count fiber. Don’t just cut sugar-replace it with whole fruit. Don’t just exercise-move daily. Walking 10,000 steps a day improves liver fat more than intense workouts for people with metabolic issues.What Doesn’t Work (And Why)
Intermittent fasting gets a lot of buzz on Reddit, and yes-some people report feeling better. But the science is mixed. A 5:2 diet (eating normally 5 days, cutting calories 2 days) can help with weight loss, but it doesn’t fix gut dysbiosis on its own. If you’re eating junk food on your “normal” days, your liver doesn’t care about your fasting window. Fecal microbiota transplants (FMT) sound like sci-fi, and they’re being studied. But right now, they’re experimental. A 2022 pilot study showed minor improvements in liver enzymes-but no change in liver tissue. Not worth the cost or risk yet. And don’t fall for miracle supplements. No pill can replace a real diet. Probiotics are helpful, but they’re not a substitute for vegetables. Fiber supplements won’t fix your gut if you’re still drinking soda.
What to Do Right Now
You don’t need a fancy plan. Start here:- Swap one sugary drink a day for water, tea, or sparkling water with lemon. That’s 30-50 grams of fructose gone.
- Add one serving of fiber-rich food at every meal-beans in your salad, oats for breakfast, an apple with lunch.
- Use olive oil instead of butter or vegetable oil for cooking.
- Take a daily probiotic with at least 10 billion CFUs of Lactobacillus and Bifidobacterium strains. Look for ones with clinical studies on NAFLD.
- Walk 30 minutes a day-no gym needed. Just move.
What’s Next for NAFLD Treatment
The field is changing fast. In January 2024, doctors officially switched from calling it NAFLD to MASLD-because it’s not just about what you don’t drink. It’s about what your body can’t handle: sugar, fat, and poor gut health. New drugs are coming. Vedanta Biosciences is testing a pill with 11 specific bacteria designed to activate liver-protecting pathways. Early results show a 38% drop in liver fat in just 24 weeks. But these won’t be available for years. For now, the best treatment is still food. Real food. Not pills. Not shakes. Not detoxes. Just vegetables, whole grains, nuts, and lean protein-with enough movement to keep your body burning fat instead of storing it.Bottom Line
Your liver doesn’t need a miracle. It needs a better gut. And your gut needs better food. Fatty liver isn’t a life sentence. It’s a signal. Listen to it. Change your plate, move your body, and give your gut the chance to heal. You don’t need to be perfect. Just consistent. And over time, your liver will thank you.Can you reverse fatty liver without losing weight?
No-not fully. While diet and probiotics can reduce inflammation and improve gut health, liver fat only drops significantly with weight loss. Losing even 5% of your body weight improves liver fat in most people. Without weight loss, improvements are temporary and limited.
Are probiotics safe for NAFLD?
Yes, for most people. Multi-strain probiotics with Lactobacillus and Bifidobacterium are well-tolerated. Some report mild bloating at first, but it usually fades within a week. Avoid probiotics if you have a weakened immune system or severe illness. Always talk to your doctor if you’re unsure.
What foods should I avoid with fatty liver?
Avoid added sugars-especially high-fructose corn syrup in sodas, candy, and packaged snacks. Limit refined carbs like white bread, pastries, and pasta. Cut out fried foods and processed meats. Alcohol isn’t the cause, but it makes liver damage worse, so avoid it completely.
How long does it take to see results from diet changes?
You may feel better-less bloating, more energy-in 2-4 weeks. Liver enzyme levels (ALT) often drop within 8-12 weeks. Significant fat reduction in the liver usually takes 3-6 months of consistent diet and weight loss. Patience is key.
Can I take fiber supplements instead of eating vegetables?
Supplements like inulin or psyllium help, but they’re not a replacement. Whole foods provide vitamins, antioxidants, and different types of fiber that work together. Vegetables, legumes, and whole grains also help you feel full, reduce cravings, and improve gut diversity in ways supplements can’t match.
Is intermittent fasting good for NAFLD?
It can help with weight loss, but only if your eating window includes healthy foods. If you’re eating pizza and soda during your feeding window, fasting won’t help your liver. The timing matters less than the quality of what you eat. Focus on nutrient-dense meals first.
Donna Packard
December 17, 2025 AT 04:59I started swapping soda for sparkling water with lemon last month. Honestly? My bloating vanished in two weeks. I didn’t even think about my liver until now-but I feel lighter, clearer-headed. Small changes really do add up.
Thanks for the reminder that healing isn’t about perfection. Just showing up matters.
Patrick A. Ck. Trip
December 17, 2025 AT 17:45While I agree with the general thrust of this post, I must point out that the term MASLD has only recently been adopted by the American Association for the Study of Liver Diseases (AASLD) in 2023, and many clinicians still use NAFLD out of habit. The shift in nomenclature reflects a growing understanding of metabolic dysfunction, but the clinical implications remain largely unchanged.
Also, while walnuts are beneficial, their polyphenol content varies widely based on soil and processing-so don’t assume all walnuts deliver the same benefit.
Sam Clark
December 19, 2025 AT 06:32This is one of the most balanced, evidence-based summaries I’ve read on this topic. Too many articles oversimplify or overhype. The emphasis on gut-liver axis mechanics, rather than just ‘eat less sugar,’ is exactly what’s needed.
For anyone reading this: consistency trumps intensity. Walking 10,000 steps daily while eating whole foods will outperform 90 minutes of HIIT twice a week if the diet remains poor. The body heals in rhythm, not bursts.
Jessica Salgado
December 19, 2025 AT 21:31I had NAFLD diagnosed two years ago. I was terrified. I tried keto. I tried vegan. I tried fasting. Nothing stuck-until I just started adding one veggie to every meal. Not because it was a ‘diet,’ but because I was tired of feeling like a zombie after lunch.
Now I eat lentils with my eggs, broccoli with my chicken, and an apple with my tea. My ALT dropped from 98 to 34 in 5 months. No supplements. No magic. Just… more plants.
I cried when my doctor said my liver looked ‘normal.’ I didn’t even know I could feel that kind of relief.
Chris Van Horn
December 21, 2025 AT 14:21Let’s be real-this is just another ‘eat more kale’ propaganda piece disguised as science. You think your liver gives a damn about your ‘butyrate’? It cares about insulin resistance, which is caused by carbs, not fructose. You’re blaming sugar when the real villain is insulin. And probiotics? Please. That’s snake oil for people who want to feel like they’re doing something without actually changing their life.
Also, ‘walk 10,000 steps’? That’s not exercise, that’s a pedometer fantasy. Do real training-or don’t bother.
Virginia Seitz
December 21, 2025 AT 18:31Swap soda for water 🥤→💧
Add veggies 🥦
Walk every day 🚶♀️
That’s it. No drama. No pills. Just life.
My mom did this. Her liver is fine now. She’s 72. 💪❤️
amanda s
December 22, 2025 AT 13:16Why are we letting Big Pharma and Big Food dictate our health? This whole ‘MASLD’ thing is just a rebrand so they can sell more supplements. Real people don’t need ‘inulin powder’-they need real food. But you won’t hear that from the dietitians getting paid by probiotic companies.
Stop buying into this. Eat meat. Eat fat. Eat real. Your liver doesn’t need your oats.
Peter Ronai
December 22, 2025 AT 17:30Everyone’s missing the point. This isn’t about diet. It’s about epigenetics. Your gut microbiome is shaped by your mother’s birth canal, your childhood antibiotic use, and your stress levels since age 5. You can’t ‘fix’ it with walnuts and walking. That’s like trying to fix a cracked foundation by painting the walls.
And the ‘5% weight loss’ claim? That’s cherry-picked data from obese patients. What about lean NAFLD? That’s rising fast-and it has nothing to do with weight. But no one talks about that because it doesn’t fit the narrative.
Steven Lavoie
December 22, 2025 AT 19:28Chris Van Horn’s comment is unnecessarily aggressive, but he’s not entirely wrong about lean NAFLD. It’s an under-discussed subset-about 15-20% of cases. These patients aren’t overweight, but they often have visceral fat, insulin resistance, and gut dysbiosis. The same dietary principles apply, but the psychological toll is different. They feel blamed for something they ‘don’t deserve.’
This post is actually one of the most compassionate summaries I’ve seen. It doesn’t shame. It just says: here’s what works. And that’s enough.
Michael Whitaker
December 24, 2025 AT 09:20I appreciate the tone, but I must respectfully challenge the claim that ‘walking 10,000 steps improves liver fat more than intense workouts.’ The cited study had a sample size of 32, and the control group was sedentary. Resistance training, particularly high-intensity, has been shown to reduce intrahepatic lipid more effectively than aerobic exercise alone in multiple RCTs.
Also, the ‘10 billion CFUs’ recommendation is arbitrary. Dose-response data is inconsistent across strains. Some studies show benefit at 1 billion. Others require 100 billion. One size does not fit all.
Brooks Beveridge
December 24, 2025 AT 14:30Let me tell you something: healing your liver isn’t about being the most disciplined person in the room. It’s about being the most consistent.
I used to think I had to overhaul everything at once. I failed. Then I just added one thing: I started eating breakfast with oats and chia seeds. No sugar. Just water and cinnamon. That one habit led to me eating more veggies, then drinking less soda, then walking after dinner. It wasn’t a diet. It was a rhythm.
My liver enzymes normalized in 4 months. I didn’t lose 20 pounds-I lost 8. But I gained peace. That’s what this post is really about. Not science. Not supplements. Not perfection. Just… showing up for yourself, one meal at a time.
You’ve got this. Not because you’re strong. But because you’re trying.
Anu radha
December 26, 2025 AT 10:51I am from India. We have a lot of people with fatty liver here. Many think it is because of alcohol. But my uncle-he never drink. He eat too much rice, bread, sweet tea. Now his liver is bad.
I start give him dal, roti, green vegetables. He feel better. Not magic. Just food. Thank you for write this.
Donna Packard
December 26, 2025 AT 12:31Anu radha, your comment made me cry a little. Thank you for sharing. It’s the same everywhere-rice, sugar, and silence. We think we’re eating ‘normal’ food, but it’s killing us slowly.
Maybe the real miracle isn’t the walnuts or the probiotics.
It’s someone saying, ‘I see you. And I know you can do this.’