Every winter, parents in Sydney and across Australia face the same dilemma: their child is coughing, congested, and can’t sleep. The urge to reach for a bottle of children’s cough syrup is strong. But here’s the hard truth - cough and cold medicines for kids under six aren’t just ineffective. They can be dangerous.
Why These Medicines Don’t Work - And Why They’re Risky
Over-the-counter cough and cold products for young children contain ingredients like dextromethorphan, pseudoephedrine, chlorpheniramine, and guaifenesin. These were designed for adult bodies. Kids under six don’t process them the same way. Their liver enzymes - the ones that break down drugs - are still developing. By age two, a child has only about 23% of the enzyme activity an adult has to safely metabolize dextromethorphan. That means even a small dose can build up in their system and cause serious harm. The U.S. Food and Drug Administration (FDA) reviewed over 120 deaths linked to these products between 1969 and 2006. Emergency rooms saw thousands of cases - mostly in toddlers aged one to three. Side effects included rapid heart rate, seizures, extreme drowsiness, and breathing problems. In some cases, kids were given too much because parents used kitchen spoons instead of the dosing cup that came with the medicine. One study found that nearly two-thirds of dosing errors in young children happened because caregivers guessed the amount. It’s not just about mistakes. These medicines simply don’t work well in young kids. Multiple studies, including ones from the American Academy of Pediatrics and the Cochrane Collaboration, show no meaningful improvement in cough or congestion when compared to a placebo. The cough might still be there - but now your child is also drowsy, hyperactive, or struggling to breathe.What the Experts Say - And Why It’s Consistent
You’ll hear the same message from every major medical group:- The American Academy of Pediatrics says: “Cough and cold medications are not recommended for children under 4.”
- The Centers for Disease Control and Prevention (CDC) reports that children aged two to three had the highest rate of emergency visits for these drugs.
- The Mayo Clinic, Cincinnati Children’s Hospital, and Nationwide Children’s Hospital all warn against use under age four, and advise talking to a doctor before giving anything to kids aged four to six.
- The FDA’s official stance hasn’t changed since 2007: “There is no evidence these products are effective - and there is clear evidence of potential serious harm.”
What You Can Do Instead - Safe, Proven Alternatives
The good news? You don’t need medicine to help your child feel better. Here’s what actually works:- For babies under six months: Use saline nasal drops and a bulb syringe to clear mucus. Run a cool-mist humidifier in the room. Keep the baby upright during feeding to help with breathing.
- For children six months to two years: Use acetaminophen (paracetamol) if they have a fever or are in pain. Dose based on weight - 10-15 mg per kg every 4-6 hours, no more than five doses in 24 hours. Never give ibuprofen to babies under six months.
- For children one year and older: A teaspoon of honey before bed can reduce nighttime coughing. Honey coats the throat and soothes irritation. It’s as effective as some cough syrups - without the risks. (Never give honey to babies under one year - it can cause infant botulism.)
- For all ages: Keep them hydrated. Offer water, breast milk, or formula often. Warm fluids like broth can help loosen mucus. A warm bath before bed can ease congestion and calm them down.

The Hidden Danger: Double Dosing
One of the most common mistakes parents make is giving more than one medicine at a time. A child might get a cough syrup, a fever reducer, and a “nighttime cold medicine” - all at once. But many of these products contain the same active ingredient: acetaminophen. Too much acetaminophen can cause liver damage - sometimes without warning signs until it’s too late. In 2023, the FDA issued a warning about a case where a two-year-old was hospitalized after being given both a cold medicine and a separate pain reliever, each containing acetaminophen. The child ended up with acute liver failure. Always check the “Active Ingredients” section on the label. If two products list the same drug, don’t give them together. If you’re unsure, ask your pharmacist.What About “Natural” or Herbal Remedies?
Some parents turn to herbal teas, eucalyptus oils, or homeopathic drops. But these aren’t regulated like medicines. There’s no proof they work, and some can be harmful. Eucalyptus oil, for example, can cause seizures in young children if inhaled or ingested. Chamomile tea might seem safe, but it can trigger allergic reactions. Stick to what’s been tested and proven: saline, honey, hydration, and rest.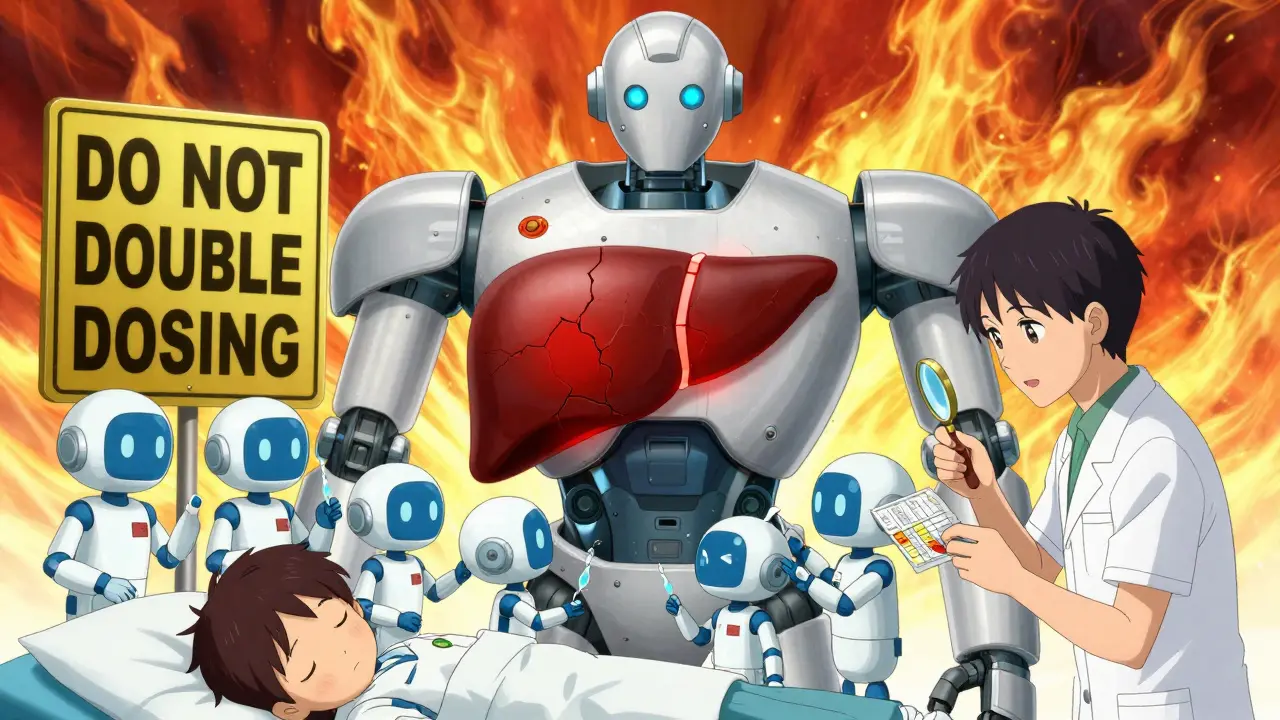
When to Call the Doctor
Most colds get better on their own in 7-10 days. But call your doctor if your child:- Has trouble breathing, fast breathing, or flaring nostrils
- Has a fever over 38°C (100.4°F) for more than three days
- Is not drinking fluids or has fewer wet diapers than usual
- Is unusually sleepy, irritable, or hard to wake up
- Has a cough that lasts more than two weeks
- Has a barking cough or wheezing - signs of croup or asthma

Neil Ellis
January 23, 2026 AT 03:42Man, I remember when my niece was two and we were up all night with that rattly cough. We almost grabbed the little purple bottle off the shelf-thank God my sister-in-law is a nurse. She said, 'Honey, that stuff is basically candy for the ER.' We did the saline drops, a humidifier, and a spoonful of honey before bed. She slept like a angel. No magic potion, just love and science. And honestly? That’s the real cure.