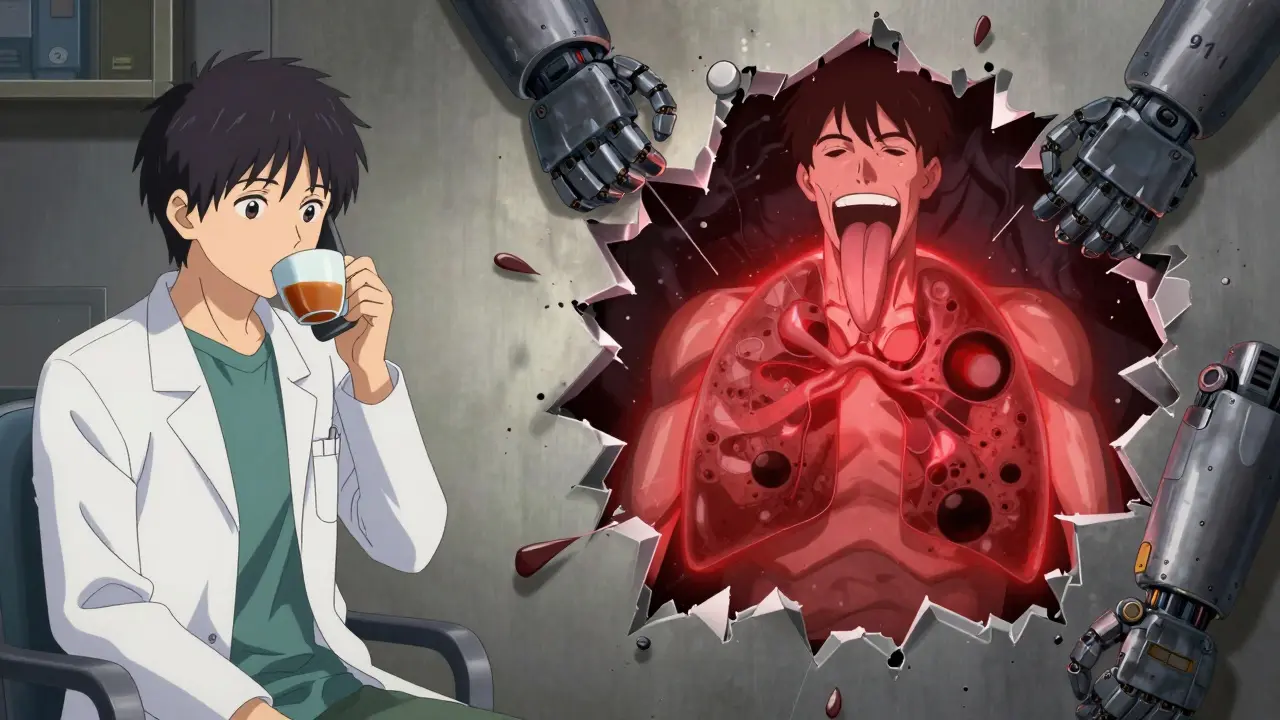
Medication Reaction Emergency Checker
This tool helps you determine if a medication reaction requires immediate emergency care (911) or can wait for a doctor's appointment. Based on FDA and Mayo Clinic guidelines.
Select symptoms you or someone is experiencing
It’s one thing to feel a little sick after taking a new pill. It’s another when your throat starts closing, your skin breaks out in hives, and you can’t catch your breath. Knowing when to call 911 instead of waiting to talk to your doctor could save your life-or someone else’s. Medication reactions aren’t all the same. Some are annoying. Others are deadly. And the difference isn’t always obvious.
Not all reactions are created equal
Most people have experienced mild side effects: a stomachache after antibiotics, a headache after a new blood pressure pill, or a bit of drowsiness from an antihistamine. These aren’t allergies. They’re side effects. Common. Expected. Usually harmless. But when your body’s immune system mistakes a drug for a threat, it triggers a real allergic reaction. And those can turn dangerous fast.
According to the FDA, about 7% of all adverse drug events are allergic reactions. That means millions of people each year react badly to medications-not just because they’re sensitive, but because their immune system is overreacting. And the symptoms? They can sneak up on you. Some show up minutes after you take the pill. Others take days. But when they hit hard, they hit hard.
Call 911 if you have these symptoms
If you or someone else has even one of these symptoms after taking medication, don’t wait. Don’t text your doctor. Don’t Google it. Call 911 right now.
- Swelling of the tongue, lips, or throat - This isn’t just puffiness. It’s a tight, growing feeling that makes swallowing or speaking hard. Dr. Mathai at Regional Hospital describes it as a "squeaky" sound when breathing-called stridor. That’s a red flag.
- Wheezing or trouble breathing - If you’re gasping, coughing, or can’t get air deep into your lungs, your airways are tightening. This is the body’s panic response. It can lead to complete blockage in minutes.
- Hives with vomiting, diarrhea, or stomach cramps - A rash alone? Maybe not urgent. But if your skin breaks out and your stomach is in revolt, your body is reacting across multiple systems. That’s the hallmark of a serious allergic reaction.
- Dizziness, fainting, or weak, fast pulse - Your heart is racing, but your blood pressure is dropping. You feel lightheaded, like you might pass out. This means your body is going into shock.
- Loss of consciousness - If someone passes out after taking a new medication, call 911 immediately. Don’t wait to see if they wake up.
The Mayo Clinic says these symptoms usually show up within an hour of taking the drug. But even if they seem to fade after 10 minutes, don’t assume it’s over. One injection of epinephrine might not be enough. Delayed reactions happen. That’s why emergency responders are trained to treat this as a ticking clock.
When to call your doctor instead
If your reaction is isolated and mild, you can usually wait until the next day to call your doctor. That doesn’t mean ignore it. It means you don’t need an ambulance.
- A simple rash without other symptoms - Just red, itchy patches on your arms or chest? No swelling, no breathing issues, no nausea? That’s likely a non-allergic skin reaction. Contact your doctor within 24 hours. They may suggest stopping the medication or switching to something else.
- Itching alone - If you’re itchy but feel fine otherwise, you can usually wait. But don’t scratch it raw. Take an antihistamine if you have one on hand (like cetirizine or loratadine), and call your doctor the next day.
- Mild nausea or diarrhea - If it’s just your stomach and nothing else, it’s probably a side effect, not an allergy. Talk to your pharmacist or doctor about whether the drug can be taken with food or if a different dosage might help.
Dr. Payel Gupta from the American College of Allergy, Asthma, and Immunology says this clearly: "A combination of symptoms like hives plus vomiting makes it much more likely that it is an allergy than nausea and vomiting on their own." One system? Likely side effect. Two or more? Time to act.

Epinephrine: Use it, don’t fear it
If you’ve been prescribed an epinephrine auto-injector (like an EpiPen), keep it with you. Always. If you think you’re having a severe reaction, use it first. Then call 911. Don’t wait to see if it gets worse.
People hesitate because they’re scared of side effects. But epinephrine is safe. The Food Allergy Research & Education organization says: "When in doubt, use it!" The risks of waiting far outweigh the risks of giving the shot. Even if you’re elderly or have heart problems, epinephrine is still the right call in anaphylaxis. The alternative is death.
And here’s the thing: even after you use epinephrine, you still need to go to the ER. One shot might not be enough. Symptoms can come back hours later. Emergency rooms are equipped to monitor you for 4 to 6 hours after a reaction. That’s not optional. That’s standard protocol.
What happens after a reaction
After surviving a serious reaction, you’ll need to see an allergist. They’ll help you figure out what caused it. Was it the antibiotic? The painkiller? The contrast dye used in imaging? Once you know, you can avoid it-and carry a medical alert card.
Also, tell every doctor you see from now on. Write it down. Put it in your phone notes. Your pharmacy needs to know. Your family needs to know. Because next time, you won’t be guessing.
Why timing matters
Every second counts. CPR Seattle says symptoms can go from mild to life-threatening in under 10 minutes. If you wait to call because you’re "not sure," you might be too late. That’s why experts say: "If you aren’t sure, call 911."
Think of it like a fire alarm. You don’t wait to see if the smoke clears. You call the fire department. Same here. If your body is screaming for help, listen.
Real numbers, real risk
In the U.S., medication reactions send about 700,000 people to the emergency room every year. The FDA logged 1.8 million reports in 2022-but experts say the real number is much higher because many reactions go unreported. Antibiotics are the most common trigger, accounting for 15% of all drug allergies. But any medication can cause a reaction.
And here’s the sobering part: 50% of fatal anaphylaxis cases happen because epinephrine was given too late. Not because it didn’t work. Because no one used it in time.
You can’t predict who will react. But you can learn to recognize the signs. And you can act before it’s too late.
