Cyclosporine Safety Monitor
Cyclosporine Safety Assessment
When you take cyclosporine after a kidney, heart, or liver transplant, you’re not just fighting rejection-you’re also managing a silent threat to your kidneys. Cyclosporine saves lives, but it can also damage the very organs it’s meant to protect. About cyclosporine nephrotoxicity affects 25% to 75% of transplant patients, and it’s one of the top reasons long-term grafts fail. The good news? You can see it coming. With the right monitoring, you can catch kidney damage early, adjust your dose, and keep your transplanted organ working for years.
Why Cyclosporine Harms the Kidneys
Cyclosporine doesn’t attack the kidney like a virus. It squeezes the blood vessels inside it. This reduces blood flow, raising pressure and starving kidney tissue. Over time, this causes scarring in tiny arteries (arteriolar hyalinosis) and swelling in tubules (tubular vacuolization). These changes start subtly-often without symptoms-until your creatinine climbs or your blood pressure spikes. The damage isn’t always permanent. If caught early and the dose is lowered, many patients see improvement within three months. But if ignored, it becomes irreversible and leads to chronic kidney disease or graft loss.What Levels Are Safe? The Numbers That Matter
Cyclosporine has a razor-thin window between working and hurting you. Too low, and your body rejects the transplant. Too high, and your kidneys pay the price. The target ranges aren’t one-size-fits-all-they change over time and by organ type.- Kidney transplant: First week: 200-400 ng/mL; Weeks 2-6: 125-275 ng/mL; Months 7-12: 100-150 ng/mL; After 1 year: 75-160 ng/mL
- Heart transplant: First 6 months: 250-350 ng/mL; After 6 months: 100-200 ng/mL
- Liver transplant: Same as heart transplant
How We Measure Cyclosporine Levels Today
Not all blood tests for cyclosporine are created equal. For years, labs used immunoassays because they were fast and cheap. But these tests often overestimate levels by 10-15% because they can’t tell the difference between cyclosporine and its metabolites. That means you might get a dose reduction when you actually need more-or worse, you’re told your levels are safe when they’re dangerously high. Today, the gold standard is liquid chromatography-tandem mass spectrometry (LC-MS/MS). Used by 92% of U.S. transplant centers in 2021, it’s accurate to 99.2%. It detects only the real drug, not its byproducts. This means your doctor gets a true picture of what’s in your blood. LC-MS/MS can measure levels as low as 5 ng/mL, making it perfect for spotting subtle changes.
When to Test: Trough Levels vs. C2 Monitoring
The old way was to draw blood just before your next dose-the trough or C0 level. But that doesn’t show the full story. Cyclosporine peaks two hours after you take it. That peak, called the C2 level, is a better predictor of how much drug your body is actually exposed to over the day. Studies show C2 monitoring cuts rejection rates by nearly 18% and reduces nephrotoxicity by over 22%. Here’s how it works:- You take your dose at 8 a.m.
- You get your blood drawn at 10 a.m.-exactly two hours later.
- Your doctor compares that C2 level to your target range.
What Else to Monitor: More Than Just Cyclosporine
You can’t just track cyclosporine levels and call it a day. Your kidneys need a full checkup. Here’s what your care team should track every visit:- Serum creatinine: Keep it under 1.5 mg/dL. Rising levels signal reduced kidney function.
- BUN-to-creatinine ratio: Should stay below 20:1. Higher numbers suggest dehydration or kidney stress.
- Magnesium: Cyclosporine pulls magnesium out of your body. Normal range: 1.7-2.2 mg/dL. Low levels can cause muscle cramps, arrhythmias, or seizures.
- Blood pressure: Target under 130/80 mmHg. High blood pressure worsens kidney damage.
- Drug interactions: Ketoconazole, erythromycin, and grapefruit juice can spike cyclosporine levels by 30-50%. Rifampin, phenytoin, and St. John’s wort can drop them by 40-60%. Always tell your doctor what else you’re taking-even over-the-counter meds.
How Often Should You Get Tested?
Testing frequency isn’t random. It’s timed to match how your body adjusts after transplant.- First month: Twice a week-your levels swing wildly as your body stabilizes.
- Months 2-6: Weekly-still high risk for rejection or toxicity.
- Months 7-12: Every two weeks-trends matter more than daily spikes.
- After 1 year: Monthly or every 6-8 weeks-if your levels and kidney function are stable.
What Can Go Wrong in Testing
Even with the best intentions, mistakes happen. Here are the top three pitfalls:- Wrong blood tube: Using a serum separator tube instead of an EDTA tube can give falsely high results by 15-20%. Always confirm the tube color-purple top for EDTA.
- Wrong timing: C2 levels must be drawn exactly two hours after your dose. If you’re late, the reading is useless. Set an alarm.
- Wrong lab: Not all labs use LC-MS/MS. Ask your transplant center which method they use. If they still use immunoassay, push for an upgrade.
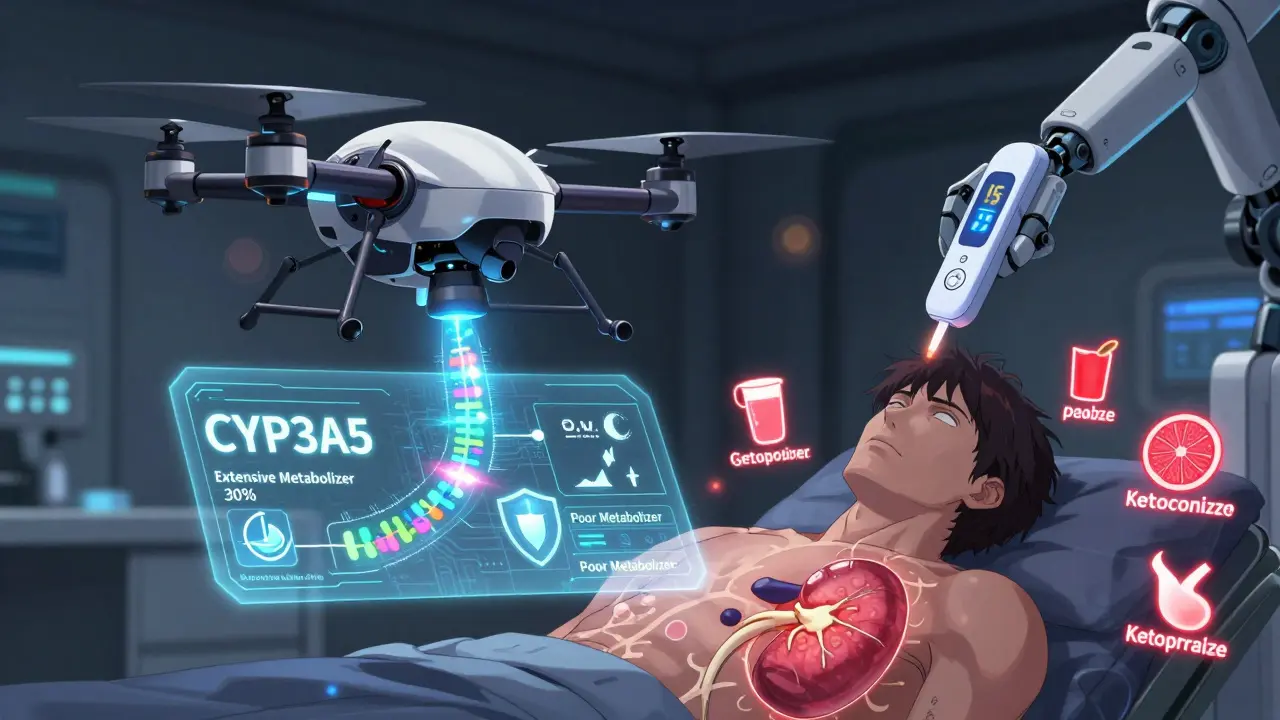
What’s Next: The Future of Monitoring
The future is faster, smarter, and more personal. Researchers are testing AI tools that predict your ideal cyclosporine dose using 17 variables-your weight, age, genetics, diet, and even your liver enzyme activity. One trial showed 89.7% accuracy in predicting the right dose without frequent blood draws. Point-of-care devices are also in Phase 3 trials. Imagine getting your cyclosporine level checked in 15 minutes with a finger-prick test-no lab needed. FDA approval is expected by late 2025. Genetic testing is already in use. If you’re a CYP3A5 extensive metabolizer, your body clears cyclosporine faster. You’ll need 30-40% more of the drug to stay in range. Testing for this once can save you years of trial and error.What You Can Do Right Now
You don’t have to wait for the future to protect your kidneys. Start today:- Know your target cyclosporine range-and ask your doctor if it’s based on C2 or trough levels.
- Always use the same lab and the same type of blood tube (EDTA).
- Set phone reminders for your blood draws and doses.
- Keep a log: date, time, dose, level, creatinine, BP, and any new meds.
- Ask: "Is my lab using LC-MS/MS?" If not, request a transfer.
- Never take new supplements or antibiotics without checking with your transplant team.
Can cyclosporine nephrotoxicity be reversed?
Yes, if caught early. Studies show that reducing the cyclosporine dose within the first few months of kidney damage can lead to partial or full recovery of kidney function within three months. The key is early detection through regular monitoring. Once scarring becomes advanced, the damage is usually permanent.
Is C2 monitoring better than trough level monitoring?
Yes, for most patients in the first year after transplant. C2 monitoring (measuring levels two hours after a dose) better reflects total drug exposure over the day. Studies show it reduces acute rejection by nearly 18% and cuts nephrotoxicity by over 22% compared to trough-only monitoring. After the first year, if your levels are stable, many centers switch back to trough testing.
Why do some labs give falsely high cyclosporine readings?
Many labs still use immunoassay tests that can’t tell the difference between cyclosporine and its metabolites. These metabolites are harmless but mimic the drug’s structure, causing the test to overestimate levels by 10-15%. This leads to unnecessary dose reductions. LC-MS/MS avoids this by detecting only the active drug.
What foods or drugs interact with cyclosporine?
Grapefruit juice, ketoconazole, erythromycin, and diltiazem can raise cyclosporine levels by 30-50%, increasing kidney risk. Rifampin, phenytoin, and St. John’s wort can lower levels by 40-60%, raising rejection risk. Even common painkillers like ibuprofen can harm your kidneys when combined with cyclosporine. Always check with your transplant team before taking anything new.
How does genetics affect cyclosporine dosing?
Your CYP3A5 gene determines how fast your body breaks down cyclosporine. If you’re an extensive metabolizer (about 15-20% of people), you clear the drug quickly and need 30-40% higher doses to reach target levels. If you’re a poor metabolizer, you need less. Genetic testing is now recommended before starting therapy to personalize dosing from day one.
Should I avoid magnesium supplements?
No-many patients on cyclosporine become magnesium deficient. Low magnesium can cause muscle cramps, irregular heartbeat, or seizures. Your doctor should check your levels every few months. If they’re low, oral magnesium supplements (like magnesium oxide or citrate) are safe and often necessary. Avoid excessive doses without medical advice.
Alex Curran
December 20, 2025 AT 02:59Been on cyclosporine for 8 years post-kidney transplant and this post nailed it. C2 monitoring saved my graft. My old center used immunoassay and kept underdosing me. Switched to LC-MS/MS and my levels jumped 30% overnight. No more rejection episodes. Also grapefruit juice is a hard no. I learned that the hard way
Lynsey Tyson
December 20, 2025 AT 04:37Just started my transplant journey and this is the most helpful thing I've read all week. I didn't even know about C2 testing. My doc just checks troughs. Gonna ask about switching. Also setting phone alarms for draws now. Thanks for laying it out so clearly
Edington Renwick
December 21, 2025 AT 04:16Wow. Just wow. This is the kind of detailed, clinically precise information that makes me wonder why anyone still uses outdated methods. LC-MS/MS isn't just better-it's the only acceptable standard. If your lab isn't using it, you're being medically negligent. And don't get me started on the 15% error margin in immunoassays. That's not a margin. That's a death sentence waiting to happen
Allison Pannabekcer
December 22, 2025 AT 18:56I'm a nurse in transplant and I see this all the time. Patients get scared when their creatinine goes up, but they don't realize it could just be dehydration or a new antibiotic. The real issue is the lack of communication. Most folks don't know to log their meds or ask about the blood tube type. This post should be handed out at every first clinic visit. Also-yes to magnesium supplements. I've seen patients have seizures because their levels dropped and no one checked. Simple fix. Don't ignore it
And for anyone new to this: your transplant team isn't trying to overwhelm you. They're trying to keep you alive. Ask questions. Write things down. You're not being a burden-you're being smart
Sarah McQuillan
December 24, 2025 AT 17:17Look, I get it. This is all very technical. But let's be real. The US is the only country that actually cares about this level of precision. In Canada, Europe, even Australia-they just use troughs and call it good. Why? Because it's cheaper. And guess what? Their graft survival rates are almost the same. So maybe we're overcomplicating this. Maybe we're spending billions on LC-MS/MS when a simple blood draw and common sense work just fine
Also, genetics? Really? I'm from the Midwest. We don't need a DNA test to know grapefruit juice is bad. Just don't eat it. Simple
Kitt Eliz
December 26, 2025 AT 16:58OMG YES 🙌 THIS IS EVERYTHING!!! C2 monitoring = GAME CHANGER 💪 LC-MS/MS is NON-NEGOTIABLE 🔬 I've been screaming this from the rooftops since 2020! And magnesium? My patient went from 1.2 to 2.1 in 2 weeks on citrate-no more cramps, no more AFib. Also, St. John’s wort is a TRAP 🚫 Don’t let your grandma’s herbal tea kill your graft. Genetic testing? DO IT. CYP3A5 status changes everything. If your doc hasn’t ordered it, FIRE THEM. You deserve precision medicine, not guesswork 🏥❤️
Aboobakar Muhammedali
December 27, 2025 AT 06:21My brother got his liver transplant in 2019. We didn't know any of this. They just gave him pills and told him to come back in a month. His creatinine went up slowly. We thought it was normal. By the time we asked about C2, it was too late. He's on dialysis now. I wish I had read this before. Please, if you're on this med, don't wait. Ask. Write it down. Set alarms. Don't be like us
anthony funes gomez
December 28, 2025 AT 01:00The entire paradigm of cyclosporine monitoring is predicated on a flawed epistemological assumption-that serum concentration correlates linearly with renal toxicity. But nephrotoxicity is a multifactorial, non-linear, time-dependent phenomenon influenced by hemodynamic, genetic, and epigenetic variables. The obsession with C2 and LC-MS/MS is reductionist. It ignores the systemic microenvironment. We are measuring a proxy. Not the pathology. Not the fibrosis. Not the endothelial dysfunction. We are quantifying a molecule. Not a process. And yet we treat the number as truth. That is not medicine. That is numerology dressed in white coats
Still. The practical utility is undeniable. So we use it. But let us not confuse utility with truth