Most people think if a drug makes them feel bad, it’s an allergy. But that’s not always true-and getting it wrong can cost you more than just discomfort. It can cost you the right treatment, increase your risk of dangerous infections, and even raise your medical bills. The truth? Only 5 to 10% of bad reactions to medications are true allergies. The other 90%? They’re side effects-predictable, common, and often manageable.
What’s Really Happening in Your Body?
A drug allergy isn’t just nausea or a rash. It’s your immune system sounding the alarm. Your body mistakes the medication for a threat-like a virus or pollen-and launches an attack. This triggers histamine release, inflammation, and sometimes life-threatening reactions. Think hives, swelling, trouble breathing, or anaphylaxis. These reactions happen because your immune system has made antibodies (usually IgE) against the drug. And if you take it again? The same response kicks in, fast and hard.
Side effects? Totally different. These are direct results of how the drug works in your body. Take statins, for example. They lower cholesterol by blocking an enzyme in your liver. But that same enzyme is also involved in muscle cell function. So, muscle aches? That’s not your immune system. That’s just the drug doing its job a little too well in the wrong place. Same with ACE inhibitors-those dry coughs? Caused by bradykinin buildup, not an immune response. No antibodies. No alarm bells. Just pharmacology.
Timing Tells the Story
When did the reaction happen? That’s your first clue.
If you took penicillin and broke out in hives within 30 minutes? That’s likely an IgE-mediated allergy. If you started amoxicillin for an ear infection and got a rash five days later? Could be an allergy-but it’s more likely a viral rash that just happened to show up while you were on the drug. Studies show 90% of kids with rashes after amoxicillin don’t have a real allergy-they had a virus.
Side effects usually show up early, too. Diarrhea from metformin? Often hits within the first 72 hours. Nausea from antibiotics? Usually fades after a few days as your gut adjusts. But if you get a rash that spreads, blisters, or comes with fever and swollen lymph nodes two to eight weeks after starting a drug? That’s DRESS syndrome-a rare but dangerous immune reaction. It needs immediate attention.
Penicillin: The Most Misunderstood Drug
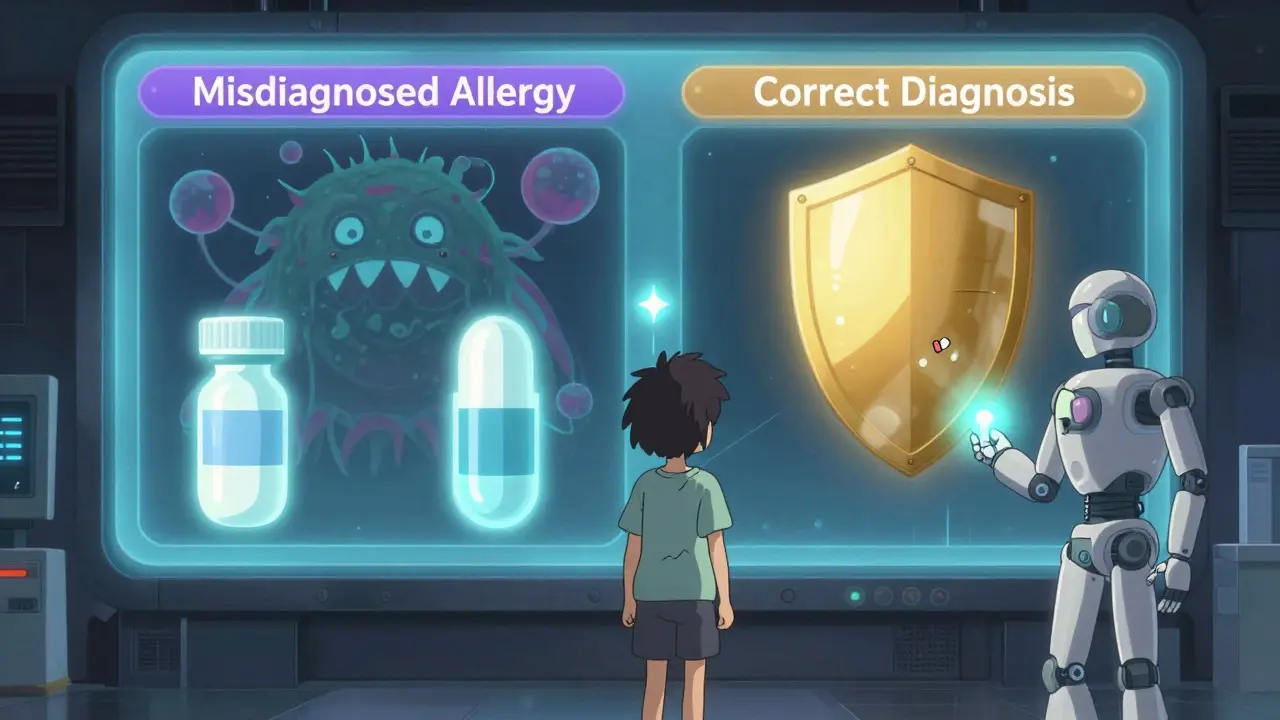
Penicillin is the poster child for this confusion. About 10% of Americans say they’re allergic. But when tested, 90% of them aren’t. Why? Because someone had a rash as a kid, or got sick after taking it, or their parent said they were allergic-and the label stuck.
Here’s the problem: if you’re labeled penicillin-allergic, doctors avoid it. They give you broader-spectrum antibiotics like vancomycin or azithromycin instead. Those drugs are more expensive. They wreck your gut bacteria. And they increase your risk of C. diff infections by 2.5 times. In hospitals, patients with a penicillin allergy label are 69% more likely to get one of these risky alternatives.
And it’s not just penicillin. Sulfa drugs, NSAIDs, and even some diabetes meds get mislabeled. A 2023 FDA review found only 14.9% of reported “drug allergies” actually met the criteria for true immune reactions. The rest? Side effects, viral rashes, or coincidences.
What Should You Do If You Think You’re Allergic?
Don’t just avoid the drug. Don’t assume you’re allergic. Get it checked.
Start with your doctor or pharmacist. Ask: “What exactly happened? When? How long did it last? Did I have trouble breathing? Was I given epinephrine?” Vague answers like “I got a rash” or “I felt sick” don’t help. Specifics do.
If there’s any chance it was a real allergy-especially if you had swelling, breathing trouble, or anaphylaxis-see an allergist. Skin testing for penicillin is highly accurate. It involves tiny pricks with the drug’s components. If both tests are negative, you’re almost certainly not allergic. Then comes a supervised oral challenge: you take a small dose under watch. Over 85% of people who’ve been told they’re allergic pass this test.
Even if you’ve never taken the drug again, testing can change your life. One patient in Sydney had a “sulfa allergy” label for 15 years. She couldn’t get antibiotics for UTIs. Her doctors kept prescribing stronger, costlier drugs. After testing, she found out she’d never been allergic. She now takes the right drug safely-and saves $3,000 a year in unnecessary prescriptions.
Why This Matters Beyond Your Own Health
This isn’t just about you. It’s about antibiotics. It’s about resistance.
When we avoid penicillin because of a mislabeled side effect, we push doctors toward broader antibiotics. That’s how superbugs like MRSA and vancomycin-resistant bacteria spread. The World Health Organization calls antibiotic resistance one of the top global health threats. And a big part of it? Misclassified drug allergies.
Health systems are catching on. In the U.S., 65% of hospitals now have formal allergy assessment programs. Pharmacists lead the charge, reviewing patient records, contacting patients, and arranging testing. In the Veterans Health Administration, these programs cut inappropriate penicillin avoidance by 80%.
Even your electronic health record is changing. New systems now require doctors to pick specific reaction types-not just “allergy.” You can’t just type “penicillin allergy.” You have to say: “hives within 1 hour,” “anaphylaxis,” or “rash with fever.” That’s helping reduce false labels by nearly half.
When to Be Worried (And When to Let It Go)
Here’s a simple guide:
- True allergy signs: Hives, swelling of lips/tongue/throat, wheezing, low blood pressure, vomiting or diarrhea with rash, anaphylaxis. These need immediate care and permanent avoidance.
- Side effects: Nausea, headache, dizziness, mild rash without other symptoms, muscle aches, dry cough, increased urination. These often improve with time, dose changes, or extra meds.
- Red flags for delayed allergy: Rash + fever + swollen glands + organ involvement (liver, kidneys). This could be DRESS or SCARs. Stop the drug and get help.
If you’re unsure, don’t guess. Talk to a professional. Even if you’ve had a reaction years ago, it’s worth revisiting. Allergies can fade. Side effects can be managed. And avoiding a safe, effective drug for no reason? That’s the real risk.
What You Can Do Today
Don’t wait for a hospital stay or an ER visit to fix this.
- Check your medical record. Look up your allergy list. What does it actually say? “Allergic to penicillin”? That’s not enough. It should say what happened.
- If you’re not sure, write down your reaction: date, drug, symptoms, how long it lasted, what you did.
- Ask your doctor: “Could this have been a side effect?”
- If it’s penicillin or sulfa, ask about allergy testing. It’s safe, fast, and covered by most insurance.
- Update your record. If you’re cleared, make sure your doctor changes your file. Tell your pharmacist too.
One simple conversation can open the door to better, safer, cheaper care. You don’t have to live with a label that doesn’t fit.
Can you outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy as a child lose the sensitivity within 10 years. Even if you were told you were allergic decades ago, you may still be able to take it safely. Testing is the only way to know for sure.
If I had a rash from amoxicillin as a kid, does that mean I’m allergic for life?
Not necessarily. Many rashes that appear while taking amoxicillin are caused by viruses-not the drug. In fact, up to 90% of these rashes in children are viral, not allergic. If you’ve never had a serious reaction like swelling or trouble breathing, it’s very likely you’re not allergic. Testing can confirm it.
Can side effects turn into allergies?
No. Side effects and allergies are two different biological processes. A side effect won’t become an allergy. But if you keep taking a drug that causes a reaction, your immune system could eventually start responding to it as a threat-especially with drugs like penicillin or sulfa. That’s why it’s important to get proper diagnosis early, not assume every bad reaction is just a side effect.
Is it safe to try a drug again if I had a mild side effect?
It depends. If the side effect was mild-like nausea, headache, or a slight rash-and didn’t involve breathing trouble or swelling, your doctor may suggest trying it again with adjustments. Maybe a lower dose, or taking it with food. But never try a drug again on your own if you had a serious reaction. Always consult a healthcare provider first.
Why do doctors still prescribe alternatives if I say I’m allergic?
Because they don’t always know the full story. If your record just says “penicillin allergy” without details, they assume the worst. That’s why it’s critical to be specific. Tell them: “I got a rash, but no swelling or breathing issues.” Or better yet, get tested and update your record. That way, they’ll know it’s safe to use the best drug for your condition.
