Imagine taking 12 pills a day - morning, noon, evening, bedtime, and then again in between. Now imagine forgetting one. Or two. Or mixing them up because the bottles look too similar. This isn’t rare. It’s everyday life for millions of older adults and people managing chronic conditions. The good news? You don’t have to live like this. Simplifying your medication regimen by reducing daily doses isn’t just convenient - it’s backed by science, and it works.
Why Fewer Doses Mean Better Adherence
People don’t miss pills because they’re lazy. They miss them because the system is broken. A study in JAMA Internal Medicine found that nearly 30% of patients take seven or more doses per day. That’s more than one pill every two hours if you’re awake. No wonder adherence drops. When you cut that down to four or fewer doses - morning, noon, evening, bedtime - adherence improves by up to 35%. That’s not magic. It’s human behavior.
Think about your own routine. You brush your teeth in the morning. You eat lunch around noon. You take your evening walk after dinner. These are anchors in your day. Medications that line up with those anchors stick. When you have to remember to take a pill at 10:15 a.m. and again at 3:45 p.m., you’re fighting your brain’s natural rhythm. Fewer doses mean fewer mental load spikes. And that’s what makes the difference.
How Fixed-Dose Combinations Cut Pill Burden
One of the most powerful tools in simplifying regimens is the fixed-dose combination (FDC). This is when two or more medications are merged into a single pill. For example, a common heart medication might combine a blood pressure drug and a cholesterol-lowering statin. Instead of two pills, you take one. That’s a 50% reduction right there.
About one-third of all successful simplifications use FDCs. They’re especially common in HIV treatment, where once-daily FDCs turned what used to be 10+ pills a day into a single tablet. Adherence jumped from 60% to over 85% in those cases. But FDCs aren’t magic bullets. They only work if the dosing schedules and drug interactions line up. You can’t just smash any two pills together. A pharmacist has to check the half-life, absorption rates, and potential side effects.
And here’s the catch: insurance doesn’t always cover them. In one Medicare study, 45% of patients were denied access to preferred FDCs because their plan only approved the older, separate versions. That’s a big barrier. But if your doctor knows the brand names and has a letter of medical necessity, they can often appeal.
Once-Daily Dosing: Not Always Possible, But When It Is, It’s Game-Changing
Not every medication can be taken once a day. Some drugs break down too fast. Others need steady levels in your blood to work. But many can - and should - be switched.
Take blood pressure meds. Many older versions required two or three doses a day. Newer extended-release versions now work for 24 hours. Same with some antidepressants, diabetes drugs like metformin XR, and even certain antibiotics. A 2018 study showed that switching HIV patients to once-daily antiretrovirals cut missed doses by more than half. No change in effectiveness. Just less hassle.
The trick? Don’t assume your current meds can’t be simplified. Ask your pharmacist: “Is there an extended-release version of this?” or “Can this be safely taken once daily?” Don’t wait for your doctor to bring it up. Pharmacists are trained to spot these opportunities. In fact, studies show that when pharmacists lead the charge, simplification happens 50% more often than when doctors try alone.
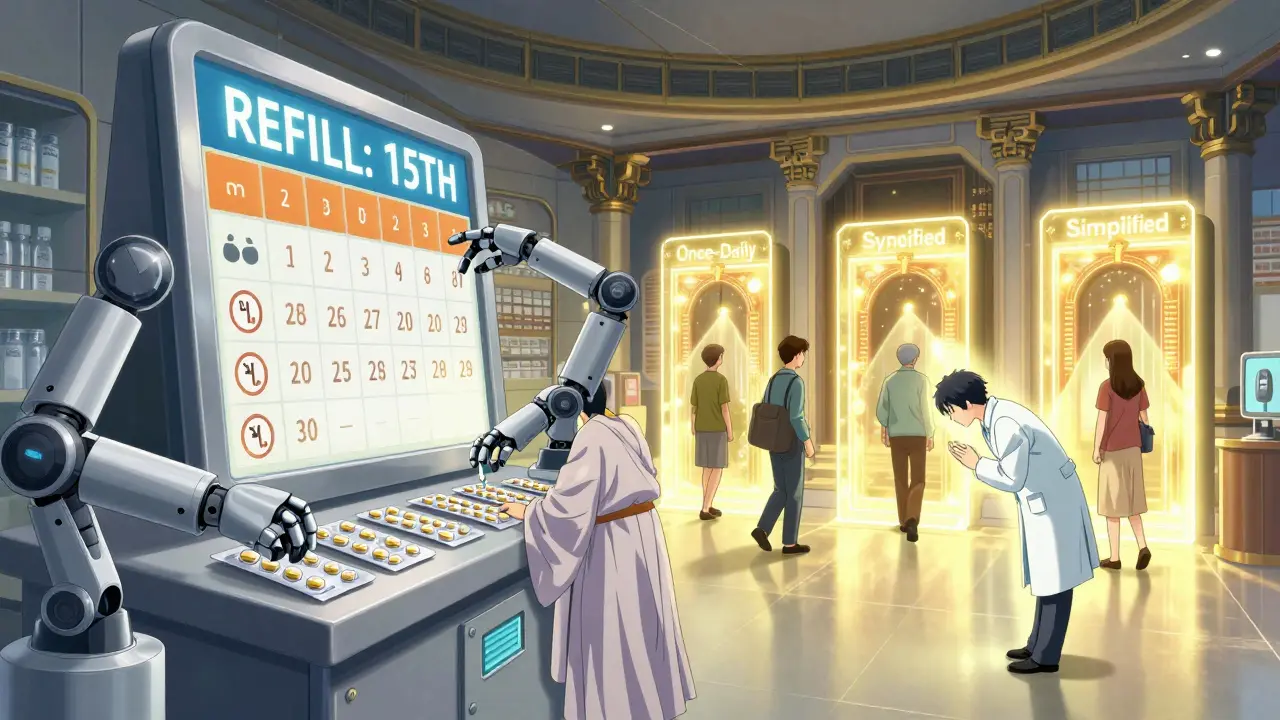
Medication Synchronization: One Day a Month, All Your Refills
Here’s something most people don’t know: your prescriptions don’t have to come due on different days. You can sync them.
Medication synchronization means all your refills are due on the same day each month - say, the 15th. That means one trip to the pharmacy instead of three. One phone call. One reminder on your phone. And no more running out of blood pressure pills because your statin refill was due a week earlier.
This isn’t just convenient. It cuts missed doses by 22% in cardiovascular patients. And it’s covered under Medicare’s medication therapy management program. All you need to do is ask your pharmacy. Most chain pharmacies and many independent ones offer this. Just tell them: “I want all my prescriptions synced to one refill date.” They’ll handle the rest - adjusting prescriptions, coordinating with your doctors, setting up reminders.

Compliance Packaging: Your Pill Organizer, Made Professional
Those little plastic boxes with four compartments - morning, noon, evening, bedtime - they’re not just for Grandma anymore. They’re a clinical tool.
Multi-dose compliance packaging (MDCP) is when your pharmacy fills your meds into a blister pack labeled by time of day. It’s especially helpful if you’re taking eight or more pills a day. One study found a 22% increase in adherence among elderly patients using these packs compared to loose bottles.
The downside? Cost. It can add $15-$20 a month to your bill. But here’s the thing: many Medicare Advantage plans cover it for high-risk patients. If you’ve had a hospital stay in the last year, or if you’re on five or more meds, ask your pharmacist: “Can I get this covered?”
And don’t try to DIY this. Putting your own meds into a box you bought at the store? Risky. You might accidentally mix drugs that shouldn’t be taken together - like blood thinners and NSAIDs. Only a pharmacist should handle this.
The 5-Step Process That Actually Works
Simplifying your regimen isn’t a one-time fix. It’s a process. And it takes teamwork.
- Medication reconciliation - Sit down with your pharmacist or doctor and list every pill, supplement, and over-the-counter drug you take. Don’t skip the aspirin or the turmeric capsules. This step takes 20-30 minutes. You’d be surprised how many discrepancies show up - an average of six per person.
- Assess your routine - When do you wake up? Eat? Go to bed? What’s your daily rhythm? This helps match meds to your life, not the other way around.
- Identify opportunities - Are any of your meds available as once-daily versions? Can any be combined? Are any no longer needed? Sometimes, a drug was prescribed years ago and never reviewed.
- Formulate a plan - Your pharmacist writes up a simplified schedule. It’s not just “take less.” It’s “take this pill with breakfast, this one at bedtime, stop this one, switch this to extended-release.”
- Coordinate implementation - Your doctor approves the changes. Your pharmacy sets up sync or packaging. You get a new schedule. You get a reminder system. You get follow-up in two weeks.
This whole process takes less than two hours total. But it’s only effective if everyone’s on the same page. If you’re doing this alone, you’ll hit walls. If your doctor doesn’t know your pharmacist is involved? Changes get ignored. Talk to both. Bring a list. Bring your pill bottles. Be loud about wanting this.
What Doesn’t Work - And Why
Not every drug can be simplified. Diabetic medications like insulin or certain hypertension drugs often need precise timing. You can’t just lump them into one dose. Some antibiotics require strict intervals to kill bacteria effectively.
And here’s a big one: people think “simpler” means “less effective.” It doesn’t. But they assume it does. That’s why 68% of pharmacists say patients misunderstand simplified regimens. They think if they’re taking fewer pills, the meds must be weaker. They skip doses “just in case.” That’s dangerous.
Also, don’t trust apps that auto-simplify without pharmacist review. Some AI tools suggest combining drugs that shouldn’t be mixed. Always have a human check it.
Real People, Real Results
One woman in Sydney, 78, was taking 14 pills a day. She’d forget which were which. She started having dizzy spells. Her pharmacist found she was taking two blood pressure meds that overlapped. One was discontinued. Two others were switched to once-daily versions. Her pills dropped to six a day - all synced to one refill date, packed into a blister pack. Her dizziness vanished. She started going out again.
Another man with HIV went from 12 pills to one. His adherence went from 60% to 96%. He got his viral load undetectable for the first time in five years.
These aren’t outliers. They’re the rule when simplification is done right.
What to Ask Your Pharmacist Today
You don’t need a degree to start this. Just three questions:
- “Can any of my medications be switched to once-daily versions?”
- “Can you sync all my refills to one day each month?”
- “Would a compliance pack help me?”
And if they say no, ask why. If they say “we don’t do that,” find a pharmacy that does. Your health is worth the extra trip.
What’s Next? AI, Smart Packs, and Better Reimbursement
The future is here. Some Medicare Advantage plans are now testing IoT-enabled pill dispensers that beep when it’s time to take your meds - and send alerts to your care team if you miss a dose. The FDA approved 12 new fixed-dose combos in 2022 alone. More are coming.
But the biggest barrier isn’t technology. It’s payment. Right now, pharmacists spend hours simplifying regimens - and get paid nothing for it. Until insurers cover medication therapy management as a standard service, progress will be slow.
That’s why your voice matters. Tell your doctor you want simplification. Tell your insurer you want coverage for compliance packs. Tell your pharmacy you’re ready to make the switch.
Simplifying your meds isn’t about cutting corners. It’s about making your life easier so your body can heal.
Can I just combine my pills myself to make fewer doses?
No. Crushing, splitting, or mixing pills without professional guidance can be dangerous. Some medications are designed to release slowly, and breaking them can cause overdose or reduce effectiveness. Others can’t be combined due to chemical reactions or absorption issues. Always consult a pharmacist before changing how you take your meds.
Will simplifying my meds lower their effectiveness?
Not if done correctly. The goal of simplification is to maintain or even improve effectiveness by increasing adherence. Studies show that when patients take fewer pills at the right times, their health outcomes improve - not because the drugs changed, but because they actually took them.
Does Medicare cover medication synchronization or compliance packaging?
Original Medicare (Parts A and B) doesn’t cover these services directly. But many Medicare Advantage plans do, especially for high-risk patients on five or more medications. Ask your plan or pharmacy if you qualify. Some also cover them under medication therapy management programs.
How do I know if I’m taking too many pills?
If you take five or more prescription medications daily, you’re considered to have polypharmacy - and your regimen is likely simplifiable. Also, if you miss doses often, feel overwhelmed, or have trouble reading labels or opening bottles, it’s time to ask for help. You don’t have to live with a confusing schedule.
How long does it take to simplify a medication regimen?
The actual planning and coordination usually takes one to two visits - about 60 to 85 minutes total. But getting prescriptions changed and new packaging or sync dates set up can take up to two weeks. Start early, and don’t wait for a crisis to act.
What if my doctor doesn’t agree with simplification?
Ask your pharmacist to write a letter of medical necessity to your doctor. Pharmacists are medication experts - and they’re often the ones who spot simplification opportunities first. If your doctor still refuses, consider getting a second opinion from a geriatrician or a pharmacist with medication therapy management certification.
Next Steps: Start Today
Don’t wait for your next appointment. Grab your pill bottles. Write down every medication you take - including vitamins and supplements. Call your pharmacy. Ask if they offer synchronization, compliance packaging, or once-daily alternatives. Bring your list. Be clear: you want fewer doses, not fewer meds.
Every pill you don’t have to remember is one less stress point in your day. And every time you take your meds correctly, you’re not just following a prescription - you’re taking back control of your health.

Jeffrey Frye
December 23, 2025 AT 14:55man i used to take 11 pills a day and i swear half of em were just for the side effects of the other half. finally got my pharmacist to sync everything to the 15th and switched two meds to XR versions. now i got 5 pills, one cup, one time. life changed. no more midnight panic attacks wondering if i took my blood pressure thing.
bharath vinay
December 25, 2025 AT 02:52they don’t want you to simplify because Big Pharma makes more money off 12 pills than one. the FDA approves these combos only when patents expire. watch how fast they pull the single-pill versions when insurance stops covering them. this is all a scam to keep you dependent.
Usha Sundar
December 27, 2025 AT 01:07i cried when my pharmacist handed me my blister pack. it was the first time in years i felt like i wasn’t failing at being sick.
claire davies
December 27, 2025 AT 03:19oh my god, this post is like a love letter to every overworked, overwhelmed, under-served person trying to stay alive on a schedule written by a robot. i’ve been a pharmacist for 18 years and i still get choked up when someone says ‘i haven’t missed a dose in six months’ after we synced their meds. it’s not about pills-it’s about dignity. being able to go out for coffee without doing a mental spreadsheet of when you took your anticoagulant. i wish every doctor had to sit in a pharmacy for a week. you’d see the real cost of ‘just take it as directed.’
Harsh Khandelwal
December 28, 2025 AT 15:29why do they even make 12-pill regimens? someone’s gotta be making bank off this chaos. i bet the pharma execs laugh when they see people juggling bottles like circus clowns.
Andy Grace
December 30, 2025 AT 08:36my dad’s on 9 meds. we did the sync thing last month. he’s been going fishing every Saturday again. didn’t realize how much he’d stopped doing things until he started again. simple stuff, really. just needed someone to ask the right questions.
Abby Polhill
December 31, 2025 AT 09:07polypharmacy risk stratification + MTM intervention = statistically significant adherence improvement (p<0.01). the real barrier is reimbursement models, not clinical feasibility. pharmacists are the underutilized frontline in medication optimization.
Austin LeBlanc
January 1, 2026 AT 03:20you’re telling me you’re too lazy to remember to take your meds? maybe you shouldn’t be on them. i’ve been on 8 pills for 15 years and i never miss one. it’s called discipline.
niharika hardikar
January 2, 2026 AT 19:25While the proposed methodology demonstrates statistical utility in adherence metrics, it neglects the pharmacoeconomic implications of fixed-dose combinations in low-resource settings. The assumption of universal pharmacist access is not generalizable across global health contexts.
Rachel Cericola
January 4, 2026 AT 04:23let me tell you what nobody says: the real win isn’t the pill count-it’s the peace. i had a patient who was taking 14 meds, couldn’t sleep, was anxious all the time. we cut it to 6, synced refills, gave her a blister pack. she called me two weeks later and said, ‘i didn’t realize i’d been holding my breath for three years.’ that’s the stuff no study measures. that’s why i do this job. don’t just ask your pharmacist about the pills-ask them how you’re *feeling*. because sometimes, the most important drug is relief.
Ajay Sangani
January 5, 2026 AT 21:02isn’t it strange that we optimize everything-phones, cars, coffee machines-but when it comes to our bodies, we just throw more pills at the problem? maybe the real simplification is asking: do we even need all these drugs? or are we just medicating symptoms of a broken system?
Pankaj Chaudhary IPS
January 6, 2026 AT 13:02as a retired officer, i know discipline matters. but discipline without support is cruelty. this post isn’t about excuses-it’s about equity. every elderly person deserves a system that works with them, not against them. thank you for writing this. i’m sharing it with my community center.
Gray Dedoiko
January 8, 2026 AT 04:54my mom’s pharmacist does the sync thing for free. she didn’t even know it was a thing until i asked. now she just grabs one bag on the 15th and goes. simple. i’m gonna do the same for my dad next week.