TB Treatment Regimen Selector
Patient Assessment
Recommended Regimen
Select patient factors above to see recommended treatment
Duration:
Cost (US, 2025): $/month
Key considerations:
Quick Takeaways
- Isoniazid remains the backbone of first‑line TB therapy but has notable neuro‑toxic and hepatotoxic risks.
- Rifampicin offers the strongest bactericidal power but induces many drug interactions.
- Ethambutol and Pyrazinamide are useful for shortening treatment duration, yet each brings distinct side‑effect profiles.
- Newer agents like Bedaquiline and Delamanid are reserved for multi‑drug‑resistant TB (MDR‑TB) and require careful cardiac monitoring.
- Choosing a regimen hinges on disease severity, resistance patterns, comorbidities, and patient adherence potential.
What is Isoniazid?
When doctors talk about standard tuberculosis (TB) therapy, Isoniazid is a first‑line antimicrobial that specifically targets Mycobacterium tuberculosis. First approved in the 1950s, it’s taken daily for six months in most uncomplicated cases. Its popularity stems from low cost, oral dosing, and proven efficacy against drug‑susceptible TB.
How Isoniazid Works: Mechanism of Action
Isoniazid inhibits the synthesis of mycolic acids, essential lipids that form the bacterial cell wall. Without a sturdy wall, the tubercle bacillus cannot survive. This mechanism is bactericidal against actively replicating bacteria but less effective on dormant loads, which is why it’s paired with other drugs that hit different bacterial targets.
Key Clinical Attributes of Isoniazid
- Typical adult dose: 5mg/kg (max 300mg) once daily.
- Side‑effects: peripheral neuropathy, hepatitis, rash, and rare sideroblastic anemia.
- Resistance: Mutations in thekatGgene or inhA promoter region can render the drug ineffective.
- Drug interactions: Minimal, but pyridoxine (vitaminB6) supplementation is recommended to prevent neuropathy, especially in diabetics or alcohol users.
- Cost (2025, US): Approximately $0.05 per tablet, making it one of the cheapest anti‑TB drugs worldwide.
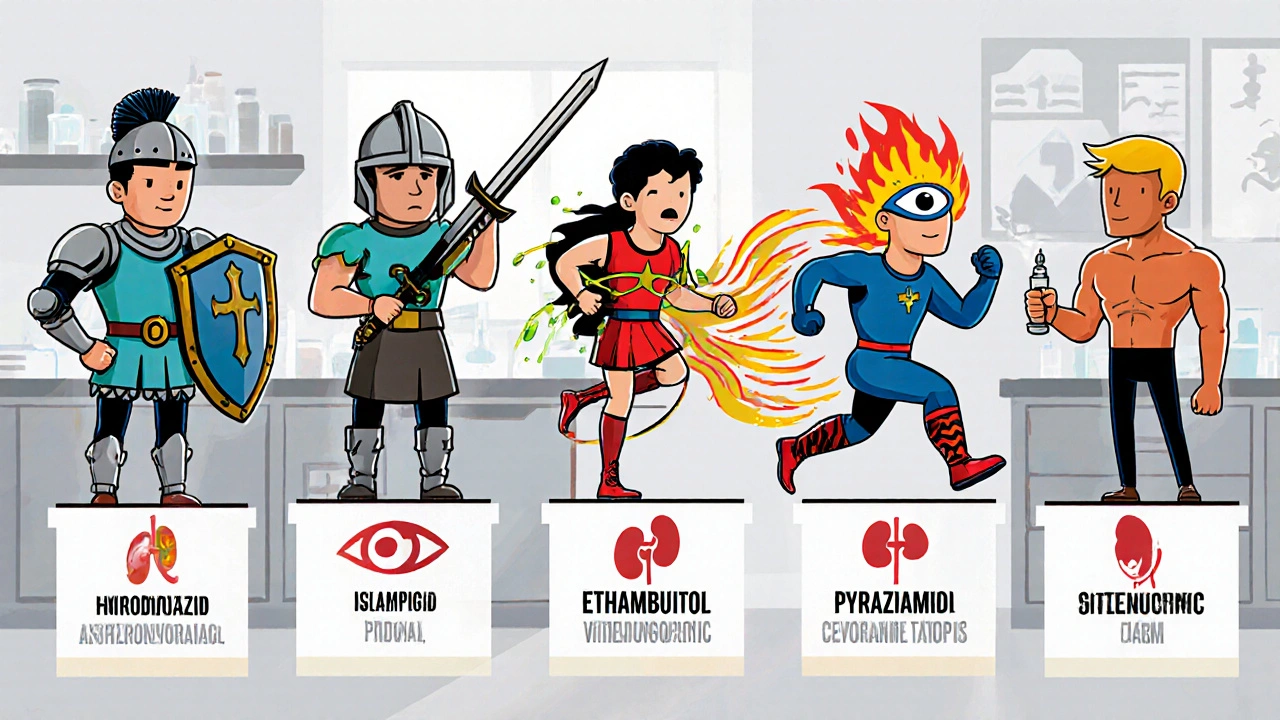
First‑Line Alternatives: Rifampicin, Ethambutol, Pyrazinamide, and Streptomycin
These four agents are the classic companions in the “RIPE” regimen (Rifampicin, Isoniazid, Pyrazinamide, Ethambutol). Below is a side‑by‑side look at how each stacks up against Isoniazid.
| Attribute | Isoniazid | Rifampicin | Ethambutol | Pyrazinamide | Streptomycin |
|---|---|---|---|---|---|
| Primary Action | Inhibits mycolic‑acid synthesis | Inhibits RNA polymerase | Disrupts cell‑wall arabinogalactan | Destroys acidic intracellular compartments | Inhibits protein synthesis (30S ribosome) |
| Typical Dose (adult) | 5mg/kg (max 300mg) daily | 10mg/kg (max 600mg) daily | 15-25mg/kg daily | 15-30mg/kg daily (first 2months) | 15mg/kg intramuscular daily (first 2months) |
| Key Side‑effects | Neuropathy, hepatitis | Hepatitis, orange body fluids, drug interactions | Optic neuritis (vision loss) | Hepatotoxicity, hyperuricemia | Ototoxicity, nephrotoxicity |
| Resistance Rate (global) | ≈10% of isolates | ≈5% of isolates | ≈3% of isolates | ≈2% of isolates | Rare (injectable‑only use) |
| Cost (US, 2025) | $0.05 per tablet | $0.12 per tablet | $0.10 per tablet | $0.15 per tablet | $0.25 per vial |
Newer Options for Drug‑Resistant TB: Bedaquiline and Delamanid
When Mycobacterium tuberculosis becomes resistant to at least isoniazid and rifampicin (MDR‑TB), clinicians turn to newer, pricier agents.
- Bedaquiline: Targets ATP synthase, leading to bacterial energy collapse. Usually given for 6months at 400mg daily (first 2weeks) then 200mg three times weekly.
- Delamanid: Inhibits mycolic‑acid synthesis via a different pathway than isoniazid. Dosage is 100mg twice daily for 6months.
Both drugs can prolong the QT interval, so baseline ECG and regular monitoring are mandatory. Their annual cost exceeds $10,000 per patient, limiting use to high‑risk cases or where WHO‑endorsed regimens demand them.
How to Choose the Right Regimen
Clinicians weigh several factors:
- Resistance profile: Drug‑susceptible TB follows the standard 6‑month RIPE course. Any resistance to isoniazid (e.g., INH‑resistant TB) often prompts substitution with fluoroquinolones or higher‑dose rifampicin.
- Patient comorbidities: Liver disease steers doctors away from isoniazid and pyrazinamide; visual impairment limits ethambutol.
- Drug interactions: Rifampicin induces CYP450 enzymes, reducing levels of antiretrovirals, oral contraceptives, and some anticoagulants.
- Adherence potential: Fixed‑dose combination tablets (RIPE) simplify regimens, reducing missed doses.
- Cost & accessibility: In low‑resource settings, affordability of isoniazid and rifampicin makes them the default.
Based on these variables, a typical decision tree looks like this: start with susceptibility testing → if both isoniazid and rifampicin are sensitive, use standard RIPE → if isoniazid resistant, replace it with a fluoroquinolone (e.g., levofloxacin) → if MDR‑TB confirmed, add bedaquiline or delamanid under specialist supervision.
Monitoring and Pitfalls
Even the best‑chosen regimen can go awry without proper follow‑up.
- Liver function: Check ALT/AST at baseline and monthly for the first two months; pause isoniazid if transaminases exceed three times the upper limit of normal.
- Neuropathy prevention: Give 25mg pyridoxine daily to anyone at risk (diabetics, pregnant women, alcohol users).
- Vision screening: Perform a red‑green color test monthly when ethambutol is part of the regimen.
- QT monitoring: For bedaquiline or delamanid, obtain an ECG before starting and then every two weeks.
Missing any of these checkpoints can lead to severe adverse events that force treatment interruption-often the biggest cause of treatment failure.
Frequently Asked Questions
Can I take isoniazid without pyridoxine?
No. Pyridoxine (vitaminB6) prevents peripheral neuropathy, especially in patients with diabetes, alcoholism, or pregnancy. Skipping it raises the risk of irreversible nerve damage.
What makes rifampicin a stronger bactericidal drug than isoniazid?
Rifampicin blocks RNA synthesis, killing both rapidly dividing and some dormant bacilli. Isoniazid mainly targets actively replicating cells, so rifampicin shortens the time needed to clear infection.
Is it safe to use streptomycin in children?
Streptomycin is generally avoided in children because of the higher risk of ototoxicity, which can affect hearing development. If an injectable is needed, alternatives like amikacin with careful monitoring are preferred.
When should I consider newer drugs like bedaquiline?
Bedaquiline is reserved for confirmed MDR‑TB or extensively drug‑resistant TB (XDR‑TB) when first‑line agents cannot be used. It’s not a substitute for isoniazid in drug‑susceptible disease.
How long should the RIPE regimen be continued?
Standard therapy lasts six months: two months of intensive phase (RIPE) followed by four months of continuation phase (usually isoniazid + rifampicin). Extensions are considered if sputum remains positive at two months.
khajohnsak Mankit
October 16, 2025 AT 15:14Reading about isoniazid feels like watching a tightrope artist who balances a feather‑light budget against a storm of neuro‑toxicity; the drug is cheap enough to buy in bulk, yet you constantly worry about the shadows it casts on nerves and livers. The paradox of such an affordable hero in the TB saga invites a philosophical reflection on how we value life‑saving simplicity versus hidden danger.
Gulam Ahmed Khan
October 23, 2025 AT 16:50Great rundown! 👍 The breakdown makes it so easy to see why isoniazid stays the workhorse, and the tip about pyridoxine is a lifesaver for anyone on the regimen. Keep the clear charts coming, they really help us stay on top of the side‑effects! 😊
John and Maria Cristina Varano
October 30, 2025 AT 17:26this is too long for me
Melissa Trebouhansingh
November 6, 2025 AT 19:02Isoniazid, as presented, is not merely a pharmacologic entity but a cultural artifact of mid‑twentieth‑century antimicrobial optimism. Its economic accessibility confers a democratic aura that belies the latent neuropathic and hepatic perils lurking beneath the surface. The table of side‑effects, while succinct, echoes centuries of clinical observation that have refined dosing strategies across continents. One must consider, however, the sociopolitical implications of deploying a drug whose adverse profile disproportionately affects marginalized populations with limited access to pyridoxine supplementation. In regions where alcohol use disorder is prevalent, the risk of peripheral neuropathy amplifies, demanding a nuanced public‑health response. Moreover, the mechanistic focus on mycolic‑acid synthesis, though elegant, reveals a singularity of bacterial vulnerability that may be circumvented by emerging resistance mutations. The comparative resistance rate of approximately ten percent underscores an evolutionary arms race that obliges clinicians to remain vigilant. Financial considerations, such as the $0.05 per tablet cost, juxtapose sharply with the hidden expenses of monitoring liver enzymes and managing adverse events. A comprehensive regimen therefore necessitates a balance of pharmacoeconomic prudence and clinical foresight. The inclusion of newer agents like bedaquiline, while clinically justified in MDR‑TB, introduces an additional layer of complexity through QT interval prolongation, thereby expanding the safety monitoring paradigm. It is also imperative to recognize that the standard RIPE model, though historically successful, is not immutable; therapeutic individualization based on comorbidities, such as HIV coinfection or diabetes, remains paramount. The recommendation for routine pyridoxine supplementation exemplifies a preventative strategy that should be universally adopted, yet implementation gaps persist. In sum, the discourse surrounding isoniazid extends beyond its antimicrobial potency to encompass ethical, economic, and epidemiologic dimensions that merit continual scholarly attention.
Brian Rice
November 13, 2025 AT 20:38Neglecting pyridoxine supplementation when prescribing isoniazid is not merely a clinical oversight; it is a moral lapse that endangers patients’ neurological health. The responsibility lies with practitioners to uphold the highest standard of care, especially for vulnerable groups such as diabetics and pregnant women.
Stan Oud
November 20, 2025 AT 22:14Sure, isoniazid is cheap- but cheap doesn't mean safe. Even though it's the backbone, you'll see more liver alerts than you’d expect. Some say the risk is overblown; I say it's under‑appreciated.
Ryan Moodley
November 27, 2025 AT 23:50Ah, the glorious era of “RIPE” regimens-how many times have we glorified a cocktail that silently steals vision or hearing? Let us not bow to tradition when the data scream for individualized therapy!
carol messum
December 5, 2025 AT 01:26I see the table and think about how each drug is like a tool in a toolbox-pick the right one for the job, and don’t forget to check the handle for cracks.
Jennifer Ramos
December 12, 2025 AT 03:02Thanks for the thorough comparison! 😀 It really helps to see the side‑effect profiles side by side. I’ll definitely share this with my clinic team.
Grover Walters
December 19, 2025 AT 04:38The inclusion of pyridoxine as a prophylactic measure reflects an understanding of the metabolic interplay between isoniazid and vitamin B6. This nuance is essential for minimizing neuropathic complications.
Amy Collins
December 26, 2025 AT 06:14From a pharmacoeconomic standpoint, the cost‑benefit ratio of isoniazid remains favorable, yet the hepatotoxicity index must be integrated into any cost‑effectiveness model.
amanda luize
January 2, 2026 AT 07:50While the grammar of the table is acceptable, the omission of a footnote on pyridoxine dosage is a glaring oversight that could mislead readers. Also, have you considered how big pharma might downplay the neuro‑toxicity to keep sales high?
Chris Morgan
January 9, 2026 AT 09:26Everyone praises isoniazid’s cheapness, but they ignore the hidden costs of monitoring. Cheap isn't always best.
Kevin Napier
January 16, 2026 AT 11:02When you start a patient on RIPE, set up a simple checklist: baseline LFTs, vitamin B6, and a schedule for monthly liver tests. This routine keeps the team on track and the patient safe.
Sherine Mary
January 23, 2026 AT 12:38The article nicely lists side‑effects, yet it fails to address the psychological burden patients feel when dealing with routine blood draws and visual tests.
Monika Kosa
January 30, 2026 AT 14:14Interesting points above, especially about the need for pyridoxine. I’ve heard some whisper that the push for cheap drugs is a deliberate move by shadowy interests to keep us dependent on routine monitoring.