It’s the same pill. Same active ingredient. Same dosage. Same manufacturer, sometimes. But if the label says generic, patients are more likely to stop taking it, feel worse, or even believe they’re having side effects - even when nothing has changed medically.
Same Medicine, Different Mindset
Picture this: two people get identical pills for their headaches. One bottle says "Ibuprofen 400 mg" with a plain white label. The other says "Advil 400 mg" with the familiar blue and white branding. Both contain exactly the same chemical. But the person with the generic label is 54% more likely to quit taking it within a week, according to a 2019 study in the European Journal of Public Health. They also report more pain, more side effects, and are more likely to reach for other pills they have lying around. This isn’t about chemistry. It’s about psychology. And it’s called the labeling effect. The idea is simple: what you call something changes how people experience it. A placebo pill labeled "brand-name" can reduce pain just as much as the real thing. But the same placebo labeled "generic"? It barely works at all.How Much Does the Label Really Matter?
In a 2016 study published in Psychology & Health, researchers gave 87 students pills labeled either "Advil" or "generic ibuprofen" - but half of them were just sugar pills. The results were startling:- People who thought they took "Advil" (even if it was sugar) reported 3.0 cm less pain on a visual scale - almost as good as the real drug.
- Those who thought they took "generic" sugar pills? Only 1.8 cm pain reduction.
- 28% of people blamed side effects on the "Advil" placebo.
- 47% blamed the same side effects on the "generic" placebo - even though it was identical.
When Belief Breaks Treatment
The World Health Organization says only about half of people with chronic illnesses take their meds as prescribed. The labeling effect makes that worse. In the same 2019 study, patients with low health literacy were nearly twice as likely to quit their generic meds. They didn’t understand bioequivalence. They didn’t know the FDA requires generics to work the same way. All they saw was "generic" and assumed it was cheaper because it was weaker. And it’s not just patients. Doctors and pharmacists feel it too. A 2022 survey found 63% of pharmacists had been asked by patients or doctors: "Is this generic really the same?" Even when they knew the answer, they had to explain it - over and over. The result? People switch back to brand-name drugs. They pay more. They skip doses. They end up in the ER because their blood pressure spiked or their depression got worse. All because of a label.
Why Does This Happen?
Our brains are wired to make quick judgments. A brand name like "Lipitor" or "Zoloft" has years of advertising, TV commercials, and word-of-mouth behind it. It feels familiar. Safe. Powerful. Generic labels? They’re often just the chemical name. Sometimes printed in tiny font on a plain white bottle. No logo. No history. No emotional connection. This isn’t rational. But it’s human. It’s the same as buying a $100 coffee mug from a fancy boutique versus a $5 one from a dollar store - even if they’re made in the same factory. The packaging, the name, the story - they change how we experience the thing itself. In medicine, that’s not just inconvenient. It’s risky.The Hidden Dangers of Labeling
There’s another layer: actual label differences. A 2020 study found that nearly half of generic drug labels had discrepancies compared to their brand-name counterparts. Not just wording - critical differences in warnings, dosage instructions, or side effect listings. Some were serious enough to cause life-threatening mistakes. Why? Because when a generic drug is approved, the manufacturer doesn’t have to copy the original label word-for-word. They just have to prove their drug works the same. So they write their own label - often based on outdated templates or incomplete data. Over time, these small differences pile up. One generic says "take with food." Another says "take on empty stomach." One warns about dizziness. Another doesn’t mention it at all. Patients get confused. Pharmacists get frustrated. Doctors get caught in the middle.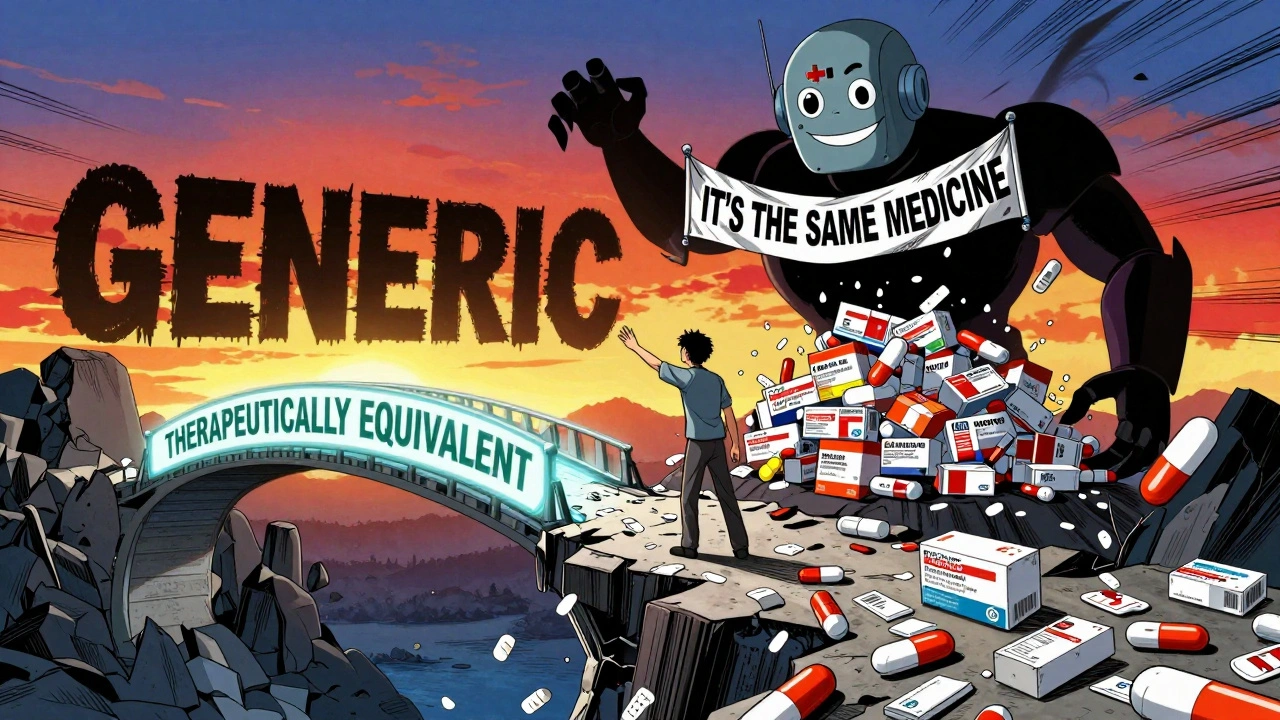
What’s Being Done?
The FDA and other regulators know this is a problem. In 2020, they launched "It’s the Same Medicine," a public campaign showing side-by-side photos of brand and generic pills with the same active ingredient. In pilot programs, patient concerns dropped by 28%. In 2023, the FDA proposed new labeling rules: generic drugs should now include phrases like "Therapeutically equivalent to [Brand Name]" right on the bottle. Early trials show this reduces discontinuation rates from 52% down to 37%. The Generic Pharmaceutical Association also launched "Generic You Can Count On" in January 2024 - a $50 million effort to rebuild trust with clear messaging, patient videos, and pharmacist training. But here’s the catch: most of these efforts are still small. They don’t reach everyone. And they don’t fix the deeper issue: the word "generic" still carries a stigma.What You Can Do
If you’re taking a generic drug:- Ask your pharmacist: "Is this the same as the brand-name version?" They can show you the FDA’s equivalence list.
- Don’t assume cheaper means worse. The FDA requires generics to be within 80-125% of the brand’s absorption rate - meaning they work the same in your body.
- If you feel worse after switching, talk to your doctor. It might be the labeling effect - not the drug.
- Look for labels that say "Therapeutically equivalent to [Brand Name]." That’s a sign the manufacturer is trying to reduce stigma.
- Don’t just say "It’s the same." Say: "This generic is FDA-approved to work exactly like [Brand Name]. Many patients save hundreds a year without losing effectiveness."
- Use the FDA’s "It’s the Same Medicine" materials in your office.
- When prescribing, consider writing "dispense as written" if you know the patient is anxious about generics.
The Bigger Picture
Generic drugs save the U.S. healthcare system $373 billion every year. That’s money that could pay for cancer treatments, mental health care, or insulin for people who can’t afford it. But if people stop taking them because they believe they’re inferior, those savings vanish. And worse - people get sicker. The labeling effect isn’t about lying. It’s about perception. And perception, in medicine, can be as powerful as a pill. The future of affordable healthcare doesn’t just depend on chemistry. It depends on how we talk about it.Calling a drug "generic" isn’t just a technical term. It’s a psychological trigger. And until we fix that, we’re not just wasting money - we’re wasting lives.

parth pandya
December 3, 2025 AT 23:23man i just switched to generic lisinopril last month and thought i was going crazy with the dizziness-turns out i was just convinced it was "weak" bc no logo. now i read the label says "therapeutically equivalent" and it actually works better. weird how your brain tricks you.
Albert Essel
December 5, 2025 AT 12:42This is one of those phenomena where science and psychology collide in the most frustrating way. The data is clear, yet the stigma persists because language shapes reality more than chemistry does. We need to rebrand "generic" as "equivalent"-not just on labels, but in public discourse.
Charles Moore
December 7, 2025 AT 05:44I’ve been a pharmacist for 18 years and I still get asked, "Is this really the same?" every single day. I show them the FDA equivalence charts, I explain bioavailability, I even let them hold the brand and generic side by side. But the word "generic" still feels like a punch in the gut to them. It’s not about the pill-it’s about the story they’ve been told.
My trick now? I say, "This is the exact same medicine your doctor prescribed, just without the marketing budget. You’re not getting less-you’re getting smarter." It helps.
Gavin Boyne
December 7, 2025 AT 21:36So let me get this straight-we’ve spent decades telling people that brand-name drugs are superior, then act shocked when they believe it? Welcome to capitalism, folks. The placebo effect is just marketing with a stethoscope.
Next up: "Organic" toilet paper that costs $12 a roll because it "feels better". Spoiler: it’s just wood pulp with a fancy label.
Rashi Taliyan
December 9, 2025 AT 20:20I cried when I switched to generic Zoloft. Not because it didn’t work-but because I felt like I was settling. Like I’d failed somehow. Like my mental health wasn’t worth the "real" thing. It took months to unlearn that shame. This post? It felt like someone finally named the ghost I’d been carrying.
Kara Bysterbusch
December 10, 2025 AT 21:55It is a profoundly disconcerting revelation that the efficacy of a pharmaceutical agent may be modulated not by its pharmacokinetic profile, but by the semiotic weight of its nomenclature. The labeling effect, as elucidated herein, represents not merely a cognitive bias, but a systemic failure of health communication infrastructure.
One must consider the ontological implications: if identity is conferred through nomenclature, then a pill labeled "generic" is ontologically diminished in the patient’s phenomenological universe, regardless of its chemical equivalence.
It is, therefore, not merely a matter of patient education, but of linguistic reclamation.
Myson Jones
December 10, 2025 AT 22:01My mom takes generic metformin and swears it gives her stomach cramps. I showed her the FDA equivalence chart. She said, "But the brand one doesn’t do that." So I asked her: "Did you ever take the brand one?" She said no. She’s been on generic since 2017. The cramps started after she read the label.
It’s not the drug. It’s the word.
bobby chandra
December 11, 2025 AT 14:54Y’all know what’s wild? The same people who’d never buy a knockoff Nike shirt will take a generic pill and blame it for their headaches. We’ll pay $200 for a sneaker because it "feels" better-but we’ll skip our blood pressure med because it came in a white bottle. We’re ridiculous.
Also, the FDA’s "It’s the Same Medicine" campaign? Genius. Why aren’t we plastering this on TV? Why aren’t pharmacies printing it on the receipt?
Archie singh
December 13, 2025 AT 07:42Pathetic. People are so dumb they think a pill’s worth is determined by its packaging. You want to feel better? Stop being a consumer and start being a patient. Take the damn pill. Stop reading blogs and Googling side effects. Your brain is your worst doctor.
Jim Schultz
December 14, 2025 AT 01:11Ohhh, so now we’re blaming the word "generic" for people’s noncompliance? Let me guess-the real issue is that people are lazy, poorly educated, and addicted to branding? Shocking. Who knew capitalism made us all gullible?
Meanwhile, the real problem is that we’ve turned medicine into a consumer product. You don’t get to pick your kidney transplant like you pick a coffee brand. But hey, at least your ibuprofen has a logo.
Kidar Saleh
December 15, 2025 AT 15:38I work in a rural clinic in Northern Ireland. Our patients are mostly elderly. Many have never heard of bioequivalence. They see "generic" and think it’s a second-rate product. We started using the FDA’s "It’s the Same Medicine" posters in the waiting room. Within two months, discontinuation rates dropped. Simple. Human. Effective.
Not everything needs to be complicated. Sometimes, a picture and a phrase are all it takes.
Chloe Madison
December 16, 2025 AT 14:59My dad took a generic statin and said he felt "flat"-like his energy was gone. We switched him back to brand. He felt better immediately. We were thrilled… until we found out the brand was a different strength. The pharmacist had misfilled it. The "brand" was actually weaker. The generic? Perfect dose.
He’s been on the generic ever since. He still thinks the brand worked better. But now he knows the truth. And he’s still mad at himself for not asking sooner.
Vincent Soldja
December 18, 2025 AT 05:52Generic drugs work. End of story.
Makenzie Keely
December 19, 2025 AT 18:30Just saw this study-mind blown. I’m a nurse, and I’ve seen patients cry because they think their generic antidepressant "isn’t real." I now keep a laminated card in my pocket: "Same medicine. Same FDA approval. Just no ads." I hand it to them. Sometimes they cry again. But this time, it’s relief.
We need more of this. Not just in clinics-in pharmacies, in ads, on insurance forms. Stop letting the word "generic" be a punchline. It’s the backbone of affordable care.