When you’re taking an SSRI antidepressant like sertraline, escitalopram, or fluoxetine, you might assume it’s safe as long as you don’t miss a dose. But what you don’t know could hurt you. Many people don’t realize that combining SSRIs with common painkillers, herbal supplements, or even other antidepressants can trigger a dangerous condition called serotonin syndrome. It doesn’t happen often-but when it does, it can land you in the ICU.
What Exactly Is Serotonin Syndrome?
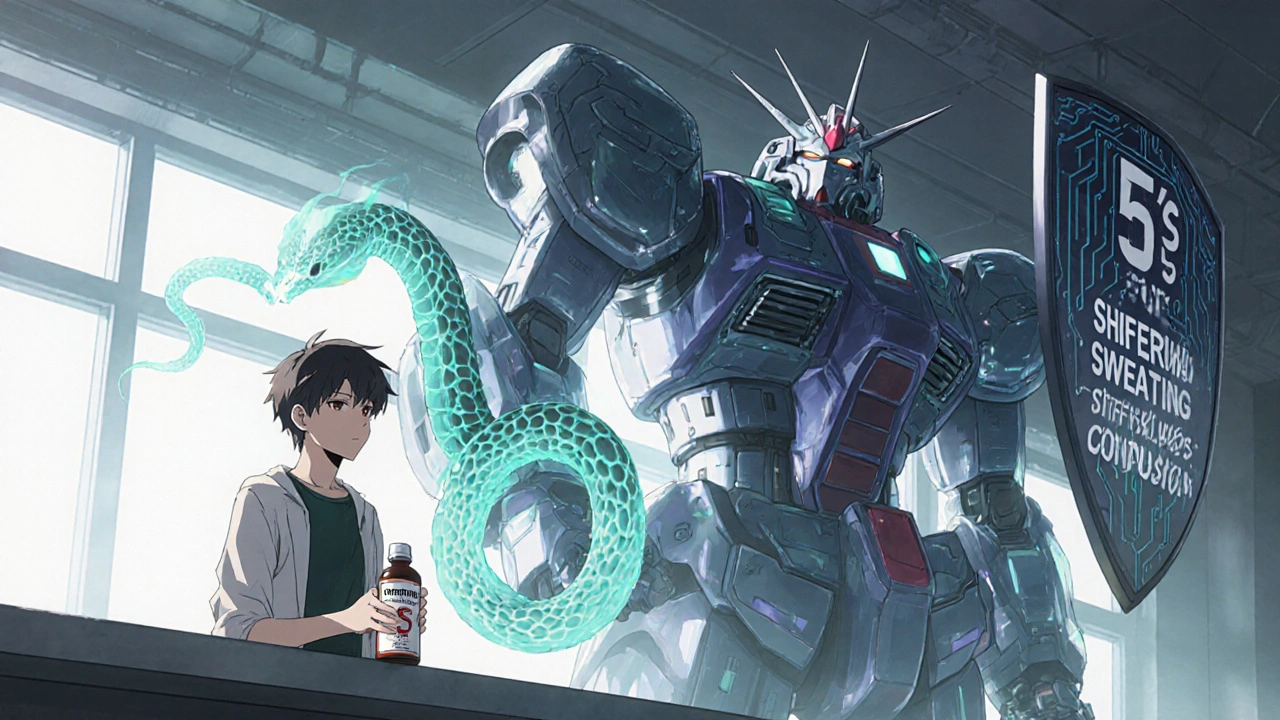
Serotonin syndrome isn’t just a side effect. It’s a medical emergency caused by too much serotonin building up in your brain. SSRIs work by blocking serotonin reabsorption, which helps lift your mood. But if another drug adds even more serotonin-or stops your body from breaking it down-your nervous system can go into overdrive.Symptoms show up fast. You might start shivering, sweating, or feeling restless. Then comes muscle stiffness, a racing heart, high fever, or confusion. In severe cases, seizures, irregular heartbeat, or loss of consciousness can happen. The Hunter Serotonin Toxicity Criteria, used by emergency doctors, say you have serotonin syndrome if you have one of these: spontaneous muscle twitches, clonus (involuntary muscle contractions) with fever or sweating, or high muscle tone with fever and eye twitching.
It’s often mistaken for the flu, heatstroke, or even a panic attack. That’s why it’s underdiagnosed. A 2020 review found only about 0.5 to 1.5 cases per 1,000 people taking SSRIs each year-but real numbers are likely higher because many mild cases go unreported.
Which Medications Raise the Risk?
Not all drug combinations are equally dangerous. Some are outright dangerous. Others are risky only under certain conditions.MAOIs are the worst. Mixing an SSRI with an MAOI like phenelzine or selegiline can be deadly. Mortality rates hit 30-50% in documented cases. That’s why doctors require a 2-week to 5-week washout period between these drugs-especially with fluoxetine, which sticks around in your system for weeks.
SNRIs like venlafaxine or duloxetine also raise the risk. A 2023 study found combining them with SSRIs increases serotonin syndrome risk by over 3 times. That’s why many prescribers avoid stacking them unless absolutely necessary.
Some opioids are silent killers. Tramadol, dextromethorphan (found in cough syrup), and pethidine (meperidine) are high-risk. They don’t just relieve pain-they also boost serotonin. A 2023 study showed tramadol combined with an SSRI increases serotonin syndrome risk by nearly 5 times. Even if you’ve taken tramadol before without issue, adding an SSRI changes the game.
On the other hand, morphine, oxycodone, and buprenorphine show little to no increased risk. If you need pain relief while on an SSRI, these are safer choices.
Linezolid, an antibiotic used for stubborn infections, is another hidden danger. It blocks serotonin breakdown. A 2022 study found patients over 65 on SSRIs who took linezolid had nearly 3 times the risk of serotonin syndrome. Many doctors don’t even think to ask about antidepressants before prescribing it.
Herbal supplements like St. John’s wort are a major red flag. People take them thinking they’re “natural” and safe. But they act like SSRIs. One user on Drugs.com reported uncontrollable shaking and confusion after just three days of mixing St. John’s wort with Prozac. ER doctors called it early serotonin syndrome.
Who’s Most at Risk?
It’s not just about what you take-it’s about who you are.Older adults are at the highest risk. Nearly 22% of Americans over 65 take an SSRI. Over 18% take an opioid for chronic pain. And 22% of seniors take five or more medications daily. That’s a recipe for accidental interactions. The FDA and CDC now warn that polypharmacy in the elderly is creating a “perfect storm” for serotonin syndrome.
People with genetic differences in liver enzymes, like CYP2D6 poor metabolizers, are also more vulnerable. Their bodies can’t break down drugs like tramadol properly, so serotonin builds up faster. Genetic testing isn’t routine-but if you’ve had bad reactions to medications before, it’s worth asking about.
People who’ve recently started or increased an SSRI dose are also at higher risk. Your body hasn’t adjusted yet. The same goes for people who’ve just added a new drug. Most serotonin syndrome cases happen within hours to days of a new combination.

What Should You Do?
You don’t have to stop your SSRI. But you do need to be smarter about what else you take.Always tell every doctor and pharmacist you’re on an SSRI. Even if they don’t ask. That includes dentists, physical therapists, and emergency staff. Many don’t think to check antidepressants when prescribing pain meds or antibiotics.
Don’t start herbal supplements without checking. St. John’s wort, 5-HTP, and tryptophan are all off-limits. Even some OTC sleep aids or cold medicines contain dextromethorphan.
Watch for the 5 S’s: Shivering, Sweating, Stiffness, Seizures (rare), and Sudden confusion. If you notice any of these after starting a new drug, stop it and call your doctor immediately. Don’t wait. Don’t assume it’s “just anxiety.”
Ask about alternatives. If you need pain relief, ask: “Is there a safer option than tramadol?” If you’re on an antibiotic, ask: “Does this interact with my antidepressant?” Most pharmacists will run a drug interaction check for free.
Keep a current medication list. Include dosages and why you take each one. Bring it to every appointment. Many hospital errors happen because staff don’t have the full picture.
How Are Doctors Responding?
The medical system is catching on. Electronic health records like Epic now flag high-risk combinations before a prescription is filled. In 2022, hospitals using these alerts cut dangerous SSRI-opioid prescriptions by 32%.Pharmacists are stepping up too. A 2023 study showed pharmacist-led medication reviews reduced serotonin syndrome events by 47% in Medicare patients. That’s not just saving money-it’s saving lives.
The FDA updated warnings in 2023 to require all antidepressants to include clear language about serotonin syndrome risk with opioids. And by 2026, a blood test called SerotoninQuant may help confirm diagnosis-something we’ve lacked for decades.
But technology can’t replace patient awareness. No alert will stop someone from grabbing a cough syrup off the shelf because they “just need to feel better.” That’s why education matters more than ever.
Real Stories, Real Consequences
One Reddit user, ‘AnxietyWarrior87,’ took sertraline for anxiety and tramadol for back pain. Within 12 hours, their body temperature spiked to 104.2°F. They developed muscle rigidity and involuntary leg spasms. They were hospitalized for three days.Another user, ‘HerbalHelp42,’ took St. John’s wort with Prozac for three days. Then came shivering, confusion, and dizziness. The ER doctor said, “You’re lucky you came in. This was early serotonin syndrome.”
These aren’t rare. The FDA’s adverse event database recorded over 1,800 serotonin syndrome cases linked to SSRIs between 2018 and 2022. Nearly 70% involved drug combinations.
And the cost? A single hospitalization averages $28,745. Many patients need ICU care. Some die.
Bottom Line
SSRIs are effective and safe when used alone. But they’re not harmless in combination. Serotonin syndrome is preventable-but only if you know the risks.You don’t need to fear your medication. But you do need to be informed. Ask questions. Check labels. Tell your providers everything. And if something feels wrong after starting a new drug-don’t brush it off. Your life could depend on it.
Can you get serotonin syndrome from just one SSRI?
It’s extremely rare. Serotonin syndrome almost always happens when an SSRI is combined with another serotonergic drug-like an SNRI, tramadol, St. John’s wort, or linezolid. Overdosing on an SSRI alone can cause it, but that’s uncommon. Most cases involve drug interactions, not single-drug use.
How long after starting a new drug does serotonin syndrome appear?
Symptoms usually start within hours to 24 hours after taking the new drug. In some cases, they can appear up to 72 hours later, especially with long-acting medications like fluoxetine. If you’ve recently added a new medication and feel unusually shaky, sweaty, or stiff, don’t wait-seek help.
Is it safe to take ibuprofen or acetaminophen with an SSRI?
Yes. Regular pain relievers like ibuprofen and acetaminophen do not increase serotonin levels and are generally safe with SSRIs. The real risks come from opioids like tramadol, certain antibiotics like linezolid, and herbal supplements like St. John’s wort. Always double-check, but standard NSAIDs and Tylenol are low-risk.
What should I do if I think I have serotonin syndrome?
Stop taking any new medications immediately and go to the nearest emergency room. Do not wait to see your doctor. Serotonin syndrome can worsen quickly. Tell the staff you’re on an SSRI and list all other drugs you’ve taken in the last 48 hours. Early treatment-like stopping the offending drug and giving supportive care-can prevent serious complications.
Can I switch from one SSRI to another safely?
It depends. Most SSRIs can be switched with a short washout period-usually just a few days. But fluoxetine is different. Because it stays in your system for weeks, you need a 5-week gap before starting another SSRI or an MAOI. Always follow your doctor’s guidance. Never switch antidepressants on your own.
Are there any new tests to diagnose serotonin syndrome?
Currently, diagnosis is based on symptoms and medication history. But a blood test called SerotoninQuant is in phase 3 trials and may be available by 2026. It measures serotonin levels directly and could help confirm cases that are unclear. Until then, doctors rely on the Hunter Criteria and clinical judgment.
Next Steps for Patients
If you’re on an SSRI:- Review your full medication list with your pharmacist every 6 months.
- Keep a printed copy of all your prescriptions and supplements in your wallet.
- Never start a new OTC medicine, herb, or supplement without checking for interactions.
- Know the 5 S’s-shivering, sweating, stiffness, seizures, sudden confusion-and act fast if they appear.
- Ask your doctor: “Could this new medication interact with my antidepressant?”
It’s not about fear. It’s about awareness. Millions take SSRIs safely every day. But a simple interaction can turn routine care into a life-threatening event. Stay informed. Stay alert. Your brain-and your body-will thank you.

Paul Baker
November 27, 2025 AT 15:46Jill Ann Hays
November 28, 2025 AT 08:29Mike Rothschild
November 29, 2025 AT 04:44Sarah McCabe
November 29, 2025 AT 21:40King Splinter
November 30, 2025 AT 09:20Michael Friend
December 1, 2025 AT 04:52Jerrod Davis
December 2, 2025 AT 12:24Dominic Fuchs
December 3, 2025 AT 08:21Asbury (Ash) Taylor
December 4, 2025 AT 14:50Kelsey Worth
December 6, 2025 AT 11:13shelly roche
December 8, 2025 AT 07:26Nirmal Jaysval
December 9, 2025 AT 22:28Emily Rose
December 10, 2025 AT 06:42