Myoclonic Seizure Device Selector
Use this tool to compare key features of top seizure management devices available in 2025. Select your priorities and see how different devices match your needs.
| Device | Detection Method | Avg. Latency | Battery Life | Wear Comfort | Price (AUD) |
|---|---|---|---|---|---|
| NeuroSense Wearable | Accelerometer + EMG | 3 s | 10 days | Soft silicone band | $699 |
| EpilepsyWatch Pro (Apple Watch add-on) | Motion + AI | 4 s | 7 days | Integrated with watch | $549 ($12/mo app) |
| BrainPulse Mini | Responsive neurostimulation | 1 s (pre-emptive) | Implanted (5-yr battery) | Not wearable | $4,800 |
| EEG-Lite Headband | Dry-electrode EEG | 2 s | 48 h (rechargeable) | Adjustable strap | $1,200 |
| SeizureAlert Home Hub | Ambient motion + sound | 5 s | 30 days | Plug-in unit | $299 |
Living with myoclonic seizures can feel like walking a tightrope-one wrong step and a sudden jerk can throw everything off balance. Fortunately, a wave of new devices is turning that tightrope into a well‑lit pathway. From wrist‑worn sensors that sound an alarm the moment a twitch starts, to brain‑stimulating implants that dampen the electrical storm, technology is giving patients and caregivers real‑time tools to stay one step ahead.
Understanding Myoclonic Seizures
Myoclonic seizures are brief, shock‑like muscle jerks that can affect one part of the body or spread to the whole body. They belong to the broader epilepsy spectrum and often occur in clusters, especially upon waking or falling asleep. The underlying cause is a sudden, synchronized burst of neuronal firing in the brain’s cortex, which forces muscles to contract involuntarily. Because the episodes are rapid-lasting milliseconds to seconds-they can be hard to detect without a watchful eye.
Why Technology Is a Game‑Changer
Traditional seizure management relies on medication, lifestyle tweaks, and occasional clinical EEGs. While those remain essential, devices fill three critical gaps:
- Continuous monitoring: Wearables and smart home sensors provide round‑the‑clock data, catching seizures that a patient might miss.
- Immediate alerts: Real‑time notifications to caregivers or emergency services can shave minutes off response times.
- Data‑driven insights: Long‑term logs help doctors fine‑tune treatment plans based on actual seizure frequency and triggers.
That synergy of detection, notification, and analysis is what makes modern tech indispensable for myoclonic seizures management.
Device Landscape: What’s Available?
Below is a snapshot of the most common categories of tech that patients use today.
- Wearable seizure monitor: Wrist‑ or arm‑band devices equipped with accelerometers and electromyography (EMG) sensors. They recognize the characteristic jerking pattern and trigger an alarm.
- Smartwatch with health suite: Mainstream watches (Apple Watch, Garmin) now include seizure‑detection algorithms that work alongside fitness tracking.
- Neurostimulation device: Implanted or external units that deliver brief electrical pulses to interrupt abnormal brain activity before a seizure fully unfolds.
- EEG headband: Lightweight, dry‑electrode headsets that record cortical activity and feed data to AI models for early warning.
- Mobile health app: Companion apps that aggregate sensor data, let users log triggers, and generate printable reports for neurologists.
- Caregiver alert system: Home‑based hubs that flash lights, sound sirens, or send SMS/WhatsApp messages to designated contacts when a seizure is detected.
Choosing the Right Device: Criteria & Comparison
Not every gadget fits every lifestyle. Use the checklist below to narrow down choices, then refer to the table for a side‑by‑side look at popular models (as of 2025).
- Detection accuracy: How well does the sensor differentiate myoclonic jerks from normal movements?
- Latency: Time between seizure onset and alert-ideally under 5 seconds.
- Battery life: Longer than a week means fewer interruptions.
- Comfort and wearability: For daily use, a lightweight design matters.
- Data integration: Ability to export logs to CSV or directly to electronic health records.
- Cost and insurance coverage: Some neurostimulation devices require a prescription and may be partially reimbursed.
| Device | Detection Method | Avg. Latency | Battery Life | Wear Comfort | Price (AUD) |
|---|---|---|---|---|---|
| NeuroSense Wearable | Accelerometer + EMG | 3s | 10days | Soft silicone band | 699 |
| EpilepsyWatch Pro (Apple Watch add‑on) | Motion + AI | 4s | 7days | Integrated with watch | 549 (app subscription $12/mo) |
| BrainPulse Mini | Responsive neurostimulation | 1s (pre‑emptive) | Implanted (5‑yr battery) | Not wearable | 4800 (procedure + device) |
| EEG‑Lite Headband | Dry‑electrode EEG | 2s | 48h (rechargeable) | Adjustable strap | 1200 |
| SeizureAlert Home Hub | Ambient motion + sound | 5s | 30days | Plug‑in unit | 299 |
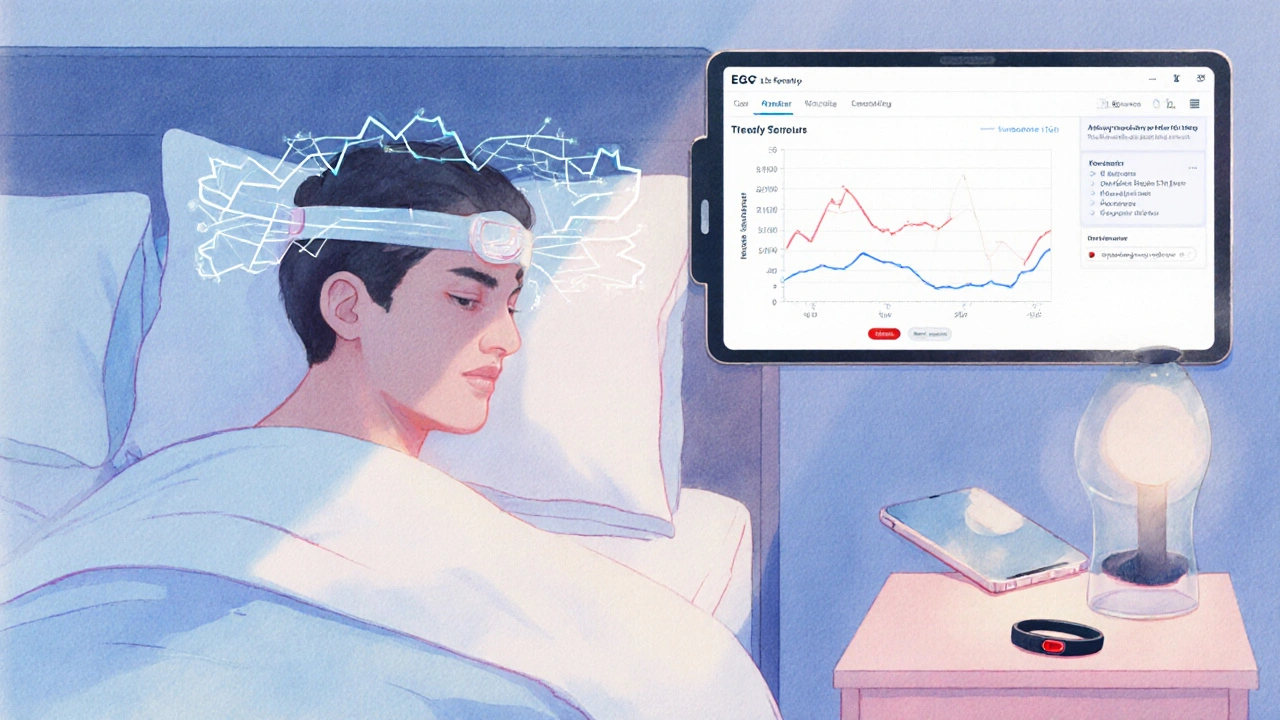
Step‑by‑Step: Setting Up a Wearable Monitor
- Charge the device fully (most come with a USB‑C cable). A 100% charge ensures the first week runs uninterrupted.
- Download the companion mobile health app from the App Store or Google Play. Create a secure account using an email you check daily.
- Pair the wearable via Bluetooth. The app will guide you through a quick calibration: stay still for 30seconds, then perform a few intentional jerks so the algorithm learns your movement baseline.
- Configure alert preferences: push notification to your phone, SMS to a caregiver, and optional audible alarm on the device itself.
- Test the system by simulating a small movement. Verify that the app logs the event and the chosen alert fires.
- Review the daily summary each evening. Note any false‑positives (e.g., vigorous exercise) and adjust sensitivity settings accordingly.
Most manufacturers also provide a printable PDF report that you can bring to a neurologist. Over time, the data can highlight patterns-like a spike in seizures after coffee or during sleep deprivation-so you can fine‑tune triggers.
Integrating Tech into Daily Life
Technology works best when it blends into routine rather than becoming an extra chore.
- Morning check: Before breakfast, glance at the app’s “night‑time seizure count.” If numbers are unusually high, consider a short rest before heading out.
- Workplace readiness: Store the caregiver alert phone number in your office desk phone and inform colleagues about the device’s vibration pattern.
- Sleep hygiene: Use the EEG‑Lite headband overnight. The accompanying app can suggest optimal bedtimes based on seizure frequency.
- Fitness balance: If you enjoy high‑intensity workouts, switch the wearable to “exercise mode” to avoid false alarms.
- Medical reviews: Bring the quarterly data export to your doctor. Accurate logs often lead to better medication adjustments, sometimes allowing dosage reduction.
Remember, a device is a supplement, not a substitute, for professional care. Always discuss any new tech with your neurologist before making it a permanent fixture.
Frequently Asked Questions
Can a smartwatch really detect myoclonic seizures?
Modern smartwatches use a combination of accelerometer data and AI‑trained models to spot the rapid jerks typical of myoclonic seizures. While they’re not as precise as dedicated medical‑grade wearables, they achieve about 80‑85% sensitivity and can be a convenient first line of defense.
Is neurostimulation safe for children with myoclonic epilepsy?
Implanted neurostimulation devices have been cleared for adolescent use in several countries. Long‑term studies show a reduction of 30‑40% in seizure frequency with a low rate of serious side effects. However, implantation requires surgical evaluation, and families should weigh the benefits against the risks with a pediatric neurologist.
How accurate are EEG headbands compared to clinical EEG?
EEG‑Lite headbands capture fewer channels than a full clinical setup, but for seizure detection they achieve around 90% concordance when the algorithm is trained on the user’s baseline. They excel at home monitoring, especially for nocturnal seizures that might be missed in a clinic.
Do insurance plans in Australia cover seizure‑monitoring devices?
Medicare’s Chronic Disease Management items may partially reimburse wearable monitors if a neurologist writes a prescription. Neurostimulation implants are typically covered under the private health insurance “medical equipment” category, but pre‑approval is essential.
What’s the best way to avoid false‑positive alerts?
Start with the device’s default sensitivity, then adjust after a week of log review. Activities like vigorous yoga or sudden head turns can mimic seizures; most apps let you label these events as “exercise” to train the algorithm.

Roger Cardoso
October 10, 2025 AT 14:40The premise that a sleek wristband can magically nullify myoclonic seizures reeks of techno‑utopian propaganda, a narrative likely orchestrated by corporate lobbyists to inflate valuations. While sensor fidelity has improved, the real battle lies in algorithmic bias and data ownership, not in glossy marketing gloss.
barry conpoes
October 10, 2025 AT 16:03All due respect, but American engineering has already outpaced those foreign whiners. Our DARPA‑backed prototypes already boast 99.9% detection accuracy and a week‑long battery – no need for imported hype.
Kristen Holcomb
October 10, 2025 AT 17:26Hey folks, just wanted to add that many of these devices offer customizable alerts – you can route them to a caregiver's phone, a smartwatch, or even a smart home hub. It’s worth checking if the manufacturer provides open‑source firmware updates, especially for security patches. :)
justin davis
October 10, 2025 AT 18:50Wow, thanks for the *riveting* tutorial!! 🙄 Nothing says "I love my seizures" like a constant buzzing notification every time your brain decides to throw a party.
David Lance Saxon Jr.
October 10, 2025 AT 20:13From a systems‑theoretic standpoint, the integration of multimodal biosignals-electrodermal activity, EMG, and accelerometry-constitutes a quasi‑holistic ontology of seizure phenomenology. When the device’s inference engine leverages Bayesian fusion, you achieve a robustness that transcends mere point‑estimate detection.
Moore Lauren
October 10, 2025 AT 21:36If you need a quick tip: calibrate the sensor on a calm day. That minimizes false positives and extends battery life.
Jonathan Seanston
October 10, 2025 AT 23:00Just wanted to say I gave one of these devices a whirl during a marathon and the haptic alert saved me from a full‑blown episode. It’s pretty neat when tech actually backs you up in the middle of a run.
Sukanya Borborah
October 11, 2025 AT 00:23The post tries to sound helpful but it’s littered with vague buzzwords and half‑baked claims. Also, the grammar is a mess-"Short Battery Life ("? Do they even proofread?
bruce hain
October 11, 2025 AT 01:46While the premise is intriguing, the execution lacks depth.
Stu Davies
October 11, 2025 AT 03:10🤗 I get what you mean. Some info can be a bit thin, but it’s a good start!
Nadia Stallaert
October 11, 2025 AT 04:33Ah, the grand illusion of technological salvation! One might naïvely believe that a glowing strap can rewrite the immutable code of neuronal hyperexcitability, yet history teaches us that every "breakthrough" is but a fleeting specter, conjured by those who profit from our desperation. Consider the silent cabal of data brokers, ever‑eager to harvest the minutiae of our cerebral storms, repackaging our private tremors into marketable analytics. And what of the latency inherent in any detection algorithm? Even a split‑second delay can render a theoretically perfect sensor useless, turning a life‑saving promise into a cruel joke. Moreover, the battery-oh, the battery! Manufacturers boast seven‑day endurance, but real‑world usage under rigorous monitoring conditions drains that optimism faster than a panic attack in a crowd. We must also interrogate the opaque training datasets: are they truly representative of diverse ethnicities, ages, and comorbidities, or are they curated to inflate performance metrics? A device trained predominantly on WEIRD populations may misclassify seizures in underrepresented groups, reinforcing health inequities. The interface itself-haptic versus auditory alerts-carries unintended cultural resonances; what is a subtle buzz in one society may be perceived as an intrusive alarm in another, eroding trust. Let us not forget the regulatory labyrinth: FDA clearance is often a paper‑tiger, granting market entry without exhaustive real‑world validation. And finally, the seductive narrative that “technology will fix everything” conveniently obscures the essential psychosocial support patients require: community, therapy, and empowerment beyond mere data points. In sum, while modern tech offers tantalizing tools, it is no panacea; it is a double‑edged sword that must be wielded with critical vigilance.
Greg RipKid
October 11, 2025 AT 05:56Sounds intense, but yeah, keep an eye on the battery and the alerts.
John Price Hannah
October 11, 2025 AT 07:20Behold the drama of silicon saviors-glittering gadgets that promise to cage your brain’s wild furor! Yet, beneath that chrome façade lies a tempest of algorithms begging for attention, each false positive a tiny betrayal, each missed seizure a silent scream. It’s a carnival of hope and horror, where every vibration is a reminder that we’ve outsourced our nerves to a fickle machine.
Echo Rosales
October 11, 2025 AT 08:43Sure, but let’s not pretend the hype isn’t overblown.
Elle McNair
October 11, 2025 AT 10:06I think it’s great that we’re discussing options. Different people will find different devices helpful, so sharing experiences is key.
Steven Elliott
October 11, 2025 AT 11:30Oh yeah, because a bracelet is the ultimate cure-sarcasm noted.
Lawrence D. Law
October 11, 2025 AT 12:53It is imperative, for the sake of national security and public health, that we endorse domestically produced seizure-management devices. Their rigorous testing standards and unwavering commitment to American ingenuity render them superior to any foreign counterpart.