When a patient starts long-term opioid therapy for chronic pain, the conversation doesn’t end with a prescription. It begins with a clear, written agreement - a opioid agreement - that sets mutual expectations between doctor and patient. These aren’t legal contracts. They’re clinical tools. And when used with real-time prescription monitoring, they can prevent harm before it happens.
What Exactly Is an Opioid Agreement?
An opioid agreement, sometimes called a pain management agreement or opioid treatment agreement, is a simple document signed by both patient and provider. It outlines what’s expected: the patient agrees to take medication exactly as prescribed, not share pills, avoid alcohol and other sedatives, and submit to random urine drug tests. The provider agrees to monitor use closely, adjust treatment if needed, and refer to addiction services if signs of misuse appear. These agreements are not about distrust. They’re about safety. Studies show that patients who sign these agreements are more likely to stick to their treatment plan and less likely to develop dependence. In fact, clinics that use them regularly see a 30% drop in emergency visits related to opioid misuse, according to data from the CDC’s 2022 Clinical Practice Guideline.Why PDMPs Are Non-Negotiable
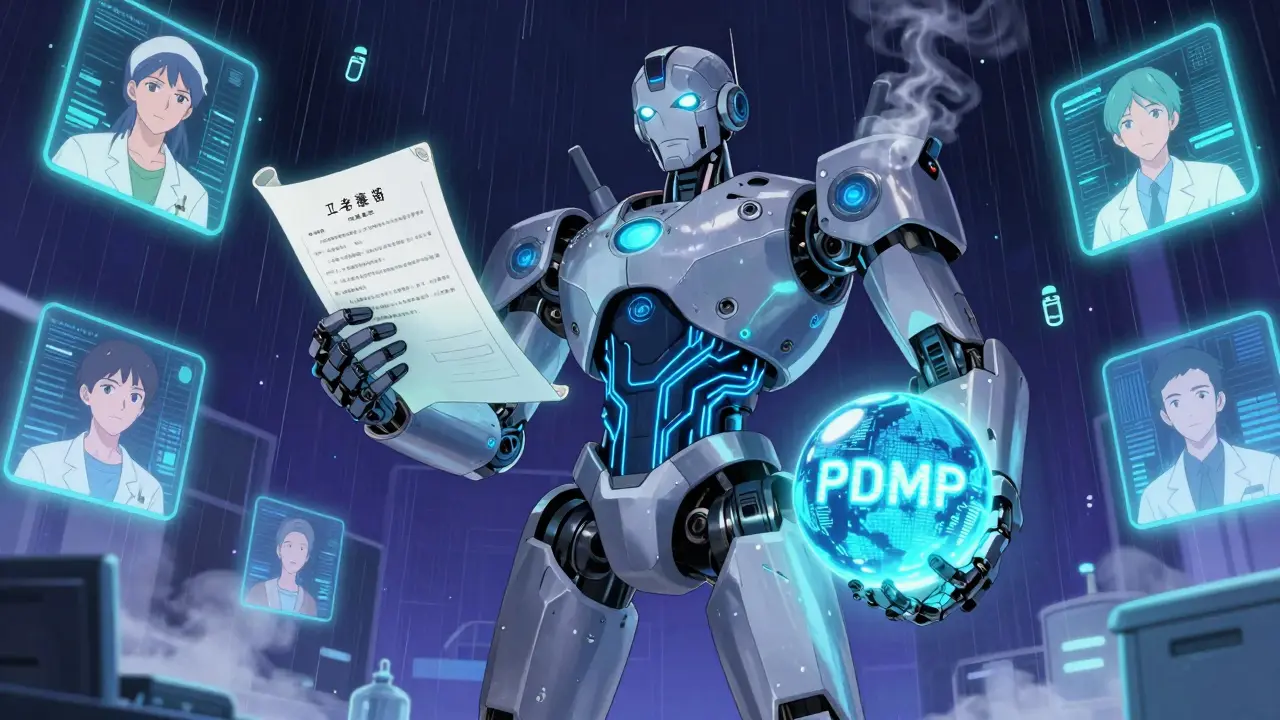
Signing an agreement is only half the job. The other half is knowing what else the patient is taking. That’s where Prescription Drug Monitoring Programs (PDMPs) come in. Every state in the U.S. now runs a PDMP - an electronic database that tracks every controlled substance prescription filled at pharmacies. It shows what drugs, how much, from which doctor, and when. In 2026, it’s not optional to check it. The CDC says you must review PDMP data before writing the first opioid prescription - and again every three months, or even before every refill. Without this check, you’re flying blind. A patient might be getting 120 mg of morphine daily from one doctor and another 80 mg from a different clinic. That’s 200 MME (morphine milligram equivalents) - well above the CDC’s recommended threshold for high-risk prescribing. A PDMP catches that. And it’s not just for opioids. It flags benzodiazepines, muscle relaxants, and other sedatives that can turn a safe dose into a deadly mix.Integration Is the Game-Changer
Ten years ago, checking a PDMP meant logging into a separate website, entering the patient’s name, date of birth, and state ID - then waiting 30 seconds to a full minute for results. Many doctors skipped it. It was too slow. Today, the best systems are built right into electronic health records (EHRs). When you open a patient’s chart in Epic, Cerner, or another major system, a PDMP alert pops up automatically. No extra login. No extra time. In clinics using integrated systems, clinicians check PDMPs in over 75% of opioid visits - up from just 12% before integration, according to AHRQ research. The difference is measurable. One study in JAMA Network Open found that integrated PDMPs led to a 2.3 times higher rate of appropriate prescribing adjustments. That means fewer overdoses, fewer hospitalizations, and more trust between patient and provider.
What the Agreement Covers - And What It Doesn’t
A good opioid agreement includes five key points:- Only one pharmacy and one prescriber for controlled substances
- No early refills unless approved in writing
- No alcohol or benzodiazepines while on opioids
- Random urine drug screens every 3-6 months
- Immediate stop if pills are lost, stolen, or sold
State Rules Vary - But the Standard Is Clear
Not every state requires PDMP checks the same way. Twenty-six states mandate a check before every opioid prescription. Others leave it to provider discretion. But the CDC’s standard doesn’t care about state lines. Their guideline says: Review PDMP before every opioid prescription - no exceptions. Even if your state doesn’t require it, your malpractice insurer might. In 2023, a survey by the Physician Misuse Liability Survey found that 82% of doctors who used PDMPs regularly felt more protected from legal risk. Those who didn’t? Forty-four percent admitted they worried about being sued for inappropriate prescribing. Also, federal rules are tightening. The SUPPORT Act of 2018 requires all Medicare Part D prescribers to register with their state PDMP. Medicaid programs in 32 states now require checks. Ignoring the system isn’t just risky - it’s becoming illegal.Real-World Problems - And How to Fix Them
No system is perfect. Here are the top three problems clinicians face:- Delayed data. Most PDMPs update once every 24 hours. If a patient fills a script at 11 p.m., you won’t see it until tomorrow. That’s dangerous if you’re deciding whether to refill today. Solution: Use the system’s “look-back” feature. If the last refill was 10 days ago and the prescription is for 30 days, you can reasonably assume it’s still in use.
- State borders. A patient from New York gets treatment in Pennsylvania. Their PDMP history isn’t automatically shared. Forty-two states now participate in the Prescription Monitoring Information Exchange (PMIX), which cuts cross-state lookup time by 63%. Always check if your state is part of it.
- False negatives. PDMPs only track pharmacy dispenses. They miss pills from a friend, a family member, or a street dealer. That’s why urine tests matter. And why you need to ask direct questions: “Have you taken any pills that weren’t prescribed to you?”
What Happens When the Agreement Is Broken?
Breaking the agreement doesn’t mean you kick the patient out. It means you have a conversation. If a patient misses a urine test, don’t assume the worst. Ask: “I noticed we haven’t had your test yet. Is something getting in the way?” Maybe they’re scared. Maybe they lost their job and can’t afford it. Maybe they’re using something you didn’t expect. If they admit to selling pills or using illicit drugs, offer help - not punishment. Refer them to a pain specialist, addiction counselor, or medication-assisted treatment program. Your goal isn’t to catch them. It’s to keep them alive. Only if they repeatedly break the agreement - and refuse help - should you stop prescribing. That’s not abandonment. It’s harm reduction.The Bigger Picture: This Isn’t Just About Opioids
Opioid agreements and PDMPs are part of a larger shift in pain management. We’re moving away from “just give the pill” to “let’s understand the whole person.” Patients with chronic pain often have depression, sleep issues, trauma, or financial stress. Opioids don’t fix those. But a structured agreement - paired with monitoring, counseling, and non-opioid treatments like physical therapy or cognitive behavioral therapy - can help them live better without risking their life. The CDC estimates that if every provider checked PDMPs before prescribing opioids, we could prevent up to 15,000 overdose deaths per year in the U.S. That’s not a guess. That’s a projection based on real data from states that made PDMP use mandatory.Final Thought: You’re Not the Bad Guy
Some patients get angry when you ask for an agreement or a urine test. They say, “You don’t trust me.” You can respond: “I trust you enough to want you to stay safe. That’s why I’m asking.” This isn’t about control. It’s about care. And the tools - agreements, PDMPs, drug tests - are there not to punish, but to protect. When used right, they save lives.Are opioid agreements legally binding?
No, opioid agreements are not legally binding contracts. They are clinical tools used to set clear expectations between patient and provider. While they don’t hold up in court, they provide documentation that the patient was informed of risks and responsibilities. This documentation can protect providers in malpractice cases and help justify treatment decisions if misuse occurs.
Do I have to check the PDMP every time I prescribe an opioid?
Yes, according to the CDC’s 2022 Clinical Practice Guideline, you should review the Prescription Drug Monitoring Program (PDMP) before every opioid prescription - whether it’s for acute pain after surgery or long-term chronic pain. This is now considered the standard of care. Even if your state doesn’t require it, failing to check increases your legal and ethical risk.
Can nurse practitioners and physician assistants use PDMPs?
Yes. As of 2023, 37 states allow nurse practitioners and physician assistants to register for and access PDMPs under their supervising provider’s license. Some states require separate registration, while others allow delegation. Always check your state’s rules, but in most cases, these providers can and should use PDMPs as part of safe prescribing.
What if my patient lives in a different state?
If your patient receives prescriptions in another state, you must check that state’s PDMP too. Forty-two states participate in the Prescription Monitoring Information Exchange (PMIX), which lets you query multiple state databases through one portal. If your state isn’t part of PMIX, you’ll need to manually log into the other state’s system. This adds time, but it’s necessary to avoid dangerous drug interactions.
How often should I do urine drug screens for patients on opioids?
For patients on long-term opioid therapy, the CDC recommends random urine drug screens every 3 to 6 months. More frequent testing (every 1-3 months) is advised for those with a history of substance use disorder, inconsistent adherence, or high-dose prescriptions. Urine tests help confirm compliance, detect illicit substances, and guide treatment changes - they’re not meant to catch patients in lies, but to support better care.
Angel Tiestos lopez
January 13, 2026 AT 01:18bro i just signed one of these agreements and my doc gave me a sticker that says ‘i trust you’ 😅 honestly? it felt weird at first… but then i realized he wasn’t doubting me-he was trying to keep me from ending up in a coffin. 🙏 opioids ain’t candy, yk?
Pankaj Singh
January 14, 2026 AT 06:33This is pure propaganda. Doctors use these ‘agreements’ to control patients and avoid liability. You think they care about your pain? They care about their insurance audits. PDMPs are surveillance tools disguised as ‘safety.’ Wake up.
Scottie Baker
January 15, 2026 AT 19:57OMG YES. I had a doc who refused to prescribe until I signed. I was pissed. Then I got my knee replaced and needed meds for 6 months. I didn’t get addicted. Didn’t OD. Didn’t lose my job. Turns out having boundaries = not dying. 🤷♂️
Angel Molano
January 16, 2026 AT 13:15If you’re not checking the PDMP before every script, you’re negligent. Period. End of story. This isn’t optional. It’s medicine.
John Tran
January 18, 2026 AT 01:11Look, I get it-agreements, PDMPs, urine tests… it all sounds like a dystopian control system, right? But here’s the thing: we live in a world where a guy in Ohio gets 200 MME from three different docs because no one talks to each other, and then he dies on his couch with a half-empty pill bottle and a Netflix queue. That’s not a tragedy-it’s a systemic failure. These tools? They’re not about punishment. They’re about interrupting the cascade before it becomes a funeral. The real question isn’t ‘why check?’ It’s ‘why didn’t we do this 20 years ago?’
Milla Masliy
January 18, 2026 AT 09:38As someone who’s been on long-term opioids for fibro, I appreciate how this breaks it down. I’ve had doctors who treated me like a criminal and others who treated me like a saint. The middle ground-clear expectations + real monitoring-is the only way forward. Also, thank you for mentioning counseling. That’s the part no one talks about.
Anny Kaettano
January 20, 2026 AT 03:22Just wanted to add: if you're a PA or NP, PLEASE get access to your state's PDMP. You're on the front lines. Your patients are counting on you. And yes-integration with EHRs is a game-changer. I used to forget to check until I got the auto-alert in Epic. Now I do it every time. No excuses.
Lance Nickie
January 21, 2026 AT 01:26PDMPs are useless. My cousin got 120 mg from one doc and 80 from another and no one caught it. Because the system updates once a day. So yeah, great tool. 🙄
sam abas
January 21, 2026 AT 23:00Let’s be real-this whole opioid agreement thing is just a legal shield for providers. The CDC doesn’t care about patients, they care about stats. And PDMPs? They’re built by tech companies who profit from healthcare data. Who’s auditing *them*? Also, ‘random’ urine tests? That’s just surveillance with a lab coat. And don’t get me started on how these systems ignore non-pharmaceutical sources like heroin or fentanyl from the street. This is performative safety. Real care would be funding mental health and housing. But that’s too expensive, right?
Clay .Haeber
January 22, 2026 AT 16:33Oh wow. A *clinical tool*. How quaint. Next you’ll tell me the FDA is just ‘a suggestion box’ and penicillin is ‘a gentle nudge toward wellness.’ You people really think slapping a signature on a form and running a 24-hour-old database check makes you a healer? You’re not doctors-you’re compliance automatons with stethoscopes. Meanwhile, real pain patients are getting abandoned because you’re too scared to prescribe without a 17-page waiver. Bravo. 🎉
Priyanka Kumari
January 24, 2026 AT 00:10As an NP in India, I’ve seen how opioid misuse is less common here-but the principles of trust, monitoring, and collaboration? Universal. We use similar agreements for benzodiazepines and psychotropics. The key isn’t the form-it’s the conversation. And yes, integrating systems saves lives. Thank you for writing this.
Avneet Singh
January 25, 2026 AT 20:47PDMPs are statistically insignificant. The CDC’s 30% reduction claim is based on cherry-picked clinic data. Real-world adherence is under 40%. Also, ‘morphine milligram equivalents’ is a flawed metric-doesn’t account for pharmacokinetics. This is evidence-free policy dressed in jargon.
Adam Vella
January 27, 2026 AT 02:58While the intent behind opioid agreements is commendable, one must not conflate clinical best practices with regulatory compliance. The ethical imperative lies not in the documentation, but in the therapeutic alliance. The PDMP, while a useful adjunct, cannot substitute for clinical judgment. Furthermore, the assertion that 15,000 deaths could be prevented annually is extrapolative and lacks causal validation. One must remain cautious of algorithmic overreach in humanistic care.