Joint pain isn’t just a part of getting older. For millions, it’s a daily battle shaped by the exact type of arthritis they have. Two conditions-osteoarthritis and rheumatoid arthritis-make up the vast majority of cases, but they’re completely different diseases. One is wear and tear. The other is your own immune system turning against you. Getting them mixed up can mean the difference between managing pain and losing joint function forever.
What Is Osteoarthritis?
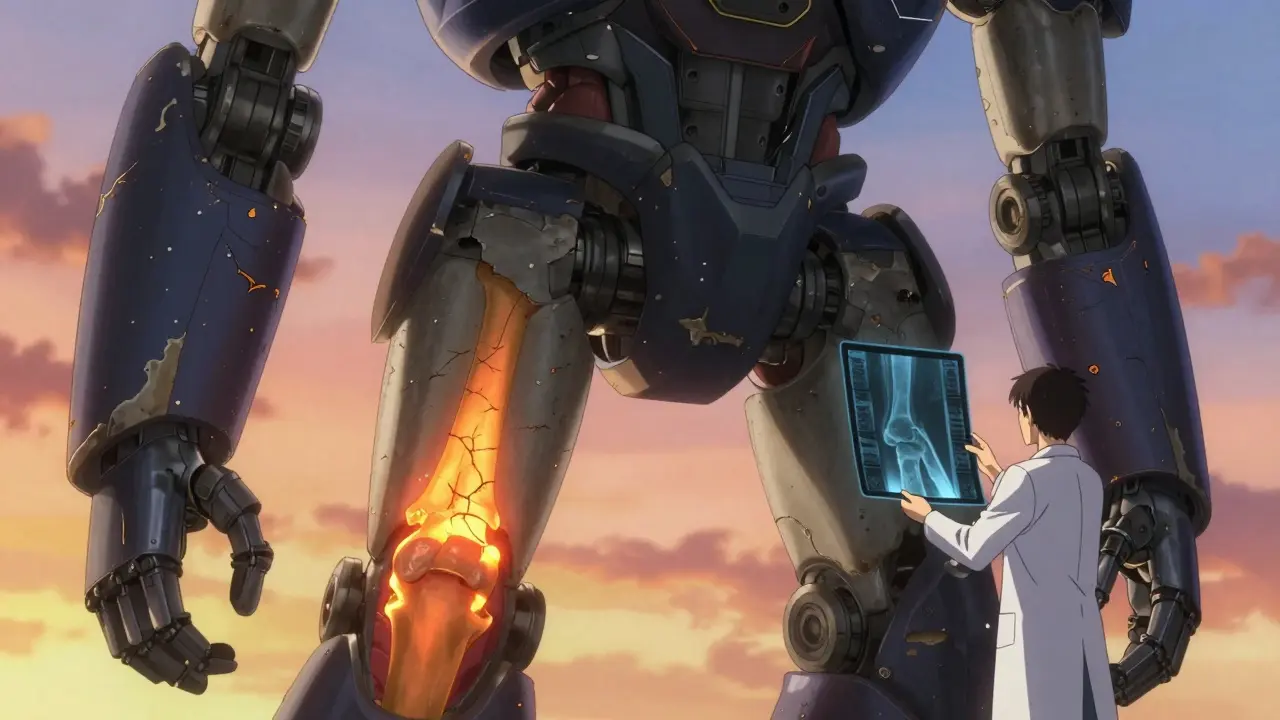
Osteoarthritis (OA) is what happens when the cushioning cartilage between your bones breaks down. Think of it like the rubber padding on a door hinge wearing thin over time. It’s not caused by infection or inflammation from your immune system. It’s mechanical. It’s stress. It’s age. It’s weight.
Most people start noticing symptoms after 50. Knees, hips, hands, and the spine are the usual suspects. You might feel a deep ache when walking up stairs or stiffness after sitting for a while. Morning stiffness? Usually less than 30 minutes. Pain gets worse with movement and improves with rest. That’s a key sign.
Hand OA often shows up in the knuckles closest to the fingertips (DIP joints) and the middle knuckles (PIP joints). You might see bony bumps there-called Heberden’s or Bouchard’s nodes. These aren’t dangerous, but they’re unmistakable. X-rays show narrowing joint space and bone spurs. No blood test can confirm it. Diagnosis is based on symptoms and imaging.
Weight matters. If you’re carrying extra pounds, your knees bear the brunt. Losing just 5 kilograms can cut knee pain in half. Physical therapy, gentle exercise, and NSAIDs like ibuprofen help manage symptoms. For advanced cases, joint replacement surgery is common-about 90% of all joint replacements in the U.S. are for OA.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) isn’t about aging or overuse. It’s an autoimmune disease. Your immune system, which normally fights germs, starts attacking the lining of your joints-the synovium. That causes swelling, heat, and pain. Left untreated, this inflammation eats away at cartilage and bone, leading to deformities.
RA can strike at any age, even in teens and young adults. It doesn’t care if you’re fit or overweight. What it does care about is genetics and smoking. Smokers are two to three times more likely to develop RA. There’s also a strong link to the HLA-DRB1 gene.
Symptoms come on faster than OA-weeks or months, not years. Morning stiffness lasts over an hour, sometimes all day. Pain isn’t just in one knee or one hand. It’s symmetrical: both wrists, both ankles, both knuckles. You’ll feel it on both sides of your body at the same time.
RA doesn’t stop at joints. It’s systemic. You might feel exhausted, run a low-grade fever, lose weight, or notice dry eyes or chest pain. Some people develop hard lumps under the skin near elbows-rheumatoid nodules. These don’t happen in OA.
Diagnosis needs blood tests. Doctors look for rheumatoid factor (RF) and anti-CCP antibodies. Ultrasound and MRI can catch early inflammation before X-rays show damage. Treatment isn’t about pain relief alone. It’s about stopping the immune attack. That means DMARDs like methotrexate, and sometimes biologics that target specific immune molecules. Starting treatment within the first three to six months is critical. Delay it, and you risk permanent joint damage.
Key Differences Between OA and RA
Here’s how they stack up side by side:
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Primary Cause | Wear and tear on cartilage | Autoimmune attack on joint lining |
| Typical Onset Age | Over 50 | Any age, including children (Juvenile RA) |
| Joint Symmetry | Usually asymmetric | Always symmetrical |
| Morning Stiffness | Less than 30 minutes | Over one hour, often all day |
| Commonly Affected Joints | Knees, hips, DIP/PIP fingers, spine | MCP joints, wrists, PIP fingers, ankles |
| Systemic Symptoms | No | Yes-fatigue, fever, weight loss, lung/eye issues |
| Diagnostic Tools | X-ray, clinical exam | Blood tests (RF, anti-CCP), ultrasound, MRI |
| Primary Treatment | Pain relief, weight loss, physical therapy, surgery | DMARDs, biologics, early aggressive therapy |
| Can It Be Stopped? | Slowed with lifestyle changes | Can go into remission with proper treatment |
One big mistake people make: assuming hand pain equals OA. If your knuckles are swollen and stiff on both hands, and your doctor doesn’t check for RA, you could be missing a critical window for treatment. RA can destroy joints in months. OA takes years.

Other Common Types of Arthritis
OA and RA aren’t the only players. There are over 100 types of arthritis. Here are three others you should know about.
Gout
Gout is sudden, intense pain in a joint-often the big toe. It’s caused by uric acid crystals building up in the joint. Attacks come out of nowhere, with redness, heat, and swelling so severe even a bedsheet can hurt. It’s linked to diet (red meat, alcohol, sugary drinks), obesity, and kidney issues. Treatment includes medications to lower uric acid and anti-inflammatories for flare-ups.
Psoriatic Arthritis
If you have psoriasis (scaly skin patches), you’re at risk. Psoriatic arthritis affects joints and the places where tendons attach to bone. It can cause sausage-like swelling in fingers or toes. Nail changes-pitting or separation-are common. It often overlaps with back pain and can mimic RA. Treatment includes DMARDs and biologics, similar to RA.
Ankylosing Spondylitis
This one targets the spine and sacroiliac joints. It causes chronic back pain and stiffness, especially in the morning. Over time, vertebrae can fuse, limiting mobility. It’s more common in men and often starts in early adulthood. A gene called HLA-B27 is strongly linked. Treatment focuses on physical therapy and biologics that block inflammation.
Why Getting the Right Diagnosis Matters
Treating OA like RA-or vice versa-can be dangerous. If you have RA and only take ibuprofen, the inflammation keeps eating your joints. You might end up needing surgery you could’ve avoided. If you have OA and are put on strong immunosuppressants, you’re exposing yourself to unnecessary risks like infections.
Doctors use a mix of history, physical exam, imaging, and blood work to tell them apart. If you’ve had joint pain for more than six weeks, especially with swelling, fatigue, or morning stiffness lasting over an hour, ask for a rheumatology referral. Don’t wait. Early RA treatment can change your life.

What You Can Do Today
Whether you have OA, RA, or another type, these steps help:
- Move regularly-even gentle walking or swimming reduces stiffness.
- Maintain a healthy weight. Every extra kilo adds pressure to your knees.
- Quit smoking. It worsens RA and slows healing.
- Protect your joints. Use larger joints to carry things. Avoid repetitive gripping.
- Track your symptoms. Note what hurts, when, and how long it lasts. Bring this to your doctor.
There’s no cure for arthritis-but there’s control. With the right diagnosis and plan, you can stay active, reduce pain, and live well.
Can osteoarthritis turn into rheumatoid arthritis?
No. Osteoarthritis and rheumatoid arthritis are completely different diseases with different causes. OA is mechanical wear and tear. RA is an autoimmune condition. One doesn’t transform into the other. But it’s possible to have both at the same time, especially as you age. That’s why proper diagnosis matters.
Is arthritis only a problem for older people?
No. While osteoarthritis is more common in older adults, rheumatoid arthritis can start in your 20s or 30s. Juvenile idiopathic arthritis affects children under 16. Gout and psoriatic arthritis also strike younger people. Age isn’t a barrier-symptoms are.
Can blood tests confirm osteoarthritis?
No. There’s no blood test for osteoarthritis. Diagnosis is based on symptoms, physical exam, and X-rays showing cartilage loss and bone spurs. Blood tests are used to rule out other types like RA or gout.
Do I need surgery if I have arthritis?
Not always. Many people manage arthritis well with exercise, weight control, and medications. Surgery-like knee or hip replacement-is usually considered only when pain severely limits daily life and other treatments have failed. For RA, joint replacement may be needed if damage is severe, but early treatment often prevents that.
Can diet help with arthritis symptoms?
Yes, especially for gout and RA. Avoiding sugary drinks, red meat, and alcohol can reduce gout flares. For RA, an anti-inflammatory diet rich in omega-3s (like fatty fish), vegetables, and whole grains may help reduce swelling. Weight loss from any diet reduces stress on joints, which helps OA.
Are natural supplements like glucosamine effective?
Evidence is mixed. Some people report relief with glucosamine or chondroitin for OA, but large studies haven’t shown strong, consistent benefits. They’re generally safe but shouldn’t replace proven treatments like exercise or medication. For RA, supplements don’t stop the immune attack-medications do.
What Comes Next?
If you’re unsure which type of arthritis you have, start with your GP. Bring a symptom journal-note which joints hurt, when it’s worst, how long stiffness lasts, and if you have other symptoms like fatigue or skin changes. Ask for a referral to a rheumatologist if RA or another autoimmune form is suspected. Don’t settle for a quick diagnosis based on age alone.
For those already diagnosed, stay engaged. New treatments for RA keep improving-JAK inhibitors, newer biologics, and personalized approaches are expanding options. For OA, research into cartilage repair and biomarkers is growing. What’s clear: early action, accurate diagnosis, and consistent management make all the difference.
Dana Termini
January 6, 2026 AT 09:03My grandma had OA in her knees and refused to believe it wasn't just 'getting old.' She started walking daily, lost 12 pounds, and now hikes with her grandkids. It's not magic-just consistent, small changes.
Don't underestimate movement. Even 20 minutes a day makes a difference.
Rachel Wermager
January 7, 2026 AT 10:49From a rheumatology perspective, the distinction between OA and RA is clinically fundamental. OA is a degenerative joint disease driven by mechanical stress and chondrocyte dysfunction, whereas RA is a systemic autoimmune disorder characterized by synovial hyperplasia, pannus formation, and cytokine-driven bone erosion-particularly via TNF-alpha, IL-6, and RANKL pathways.
Anti-CCP positivity has >95% specificity for RA, and early DMARD initiation within the 'window of opportunity' (first 12 weeks) significantly reduces radiographic progression. Delayed diagnosis correlates with irreversible joint damage and increased disability burden.
Tom Swinton
January 8, 2026 AT 08:54I know someone who was told for years it was just 'old age' until she finally saw a rheumatologist and got diagnosed with RA at 34-she was in tears because she finally had answers. It’s heartbreaking how often people get dismissed, especially women and younger folks.
It’s not just about pain-it’s about being seen. If you’ve got symmetrical swelling, morning stiffness over an hour, fatigue that doesn’t go away… don’t wait. Push for bloodwork. Push for imaging. Your future self will thank you.
Leonard Shit
January 10, 2026 AT 02:39so like… if you have arthritis and your doctor says ‘it’s just aging’… you’re probably being gaslit.
also, i once tried glucosamine. it tasted like chalk and did nothing. but hey, at least my wallet felt better.
Gabrielle Panchev
January 11, 2026 AT 06:21Actually, I’ve read multiple studies suggesting that OA isn’t purely ‘wear and tear’-there’s emerging evidence of low-grade inflammation playing a role, especially in metabolic OA. The old ‘mechanical only’ model is outdated.
And RA doesn’t always present symmetrically in early stages-some patients have asymmetric oligoarthritis before it progresses. So calling it ‘always symmetrical’ is misleading.
Also, gout isn’t just about diet-it’s heavily influenced by genetics and renal excretion efficiency. And psoriatic arthritis can mimic OA in the DIP joints, which is why imaging is critical.
And don’t even get me started on how ‘anti-inflammatory diets’ are oversold without controlled trials. Most people think ‘eat salmon’ fixes everything, but cytokine modulation isn’t that simple.
Also, HLA-B27 isn’t diagnostic-it’s just a risk factor. Many people with it never develop AS.
And why is everyone ignoring juvenile idiopathic arthritis subtypes? They’re not just ‘RA in kids.’
And the part about surgery being ‘only’ for severe OA? That’s dangerous. Some patients with advanced OA benefit from early intervention, especially if they’re active and young.
And why is no one talking about the role of gut microbiota in RA? It’s in the literature.
And why are supplements still being mentioned like they’re valid alternatives? That’s pseudoscience.
And the ‘walk more’ advice? It’s fine for knees, but what about hips with femoroacetabular impingement? Walking might make it worse.
And why is there no mention of fibromyalgia overlap? So many RA and OA patients have comorbid central sensitization.
So… yeah. This article is a good start. But it’s not the whole story.
Venkataramanan Viswanathan
January 13, 2026 AT 03:26In India, many elderly treat joint pain with turmeric paste and yoga. It helps with mild OA, but for RA, modern medicine is non-negotiable.
My uncle ignored his swollen fingers for two years-by the time he saw a doctor, his hands were deformed. He now takes methotrexate and can barely hold a spoon.
Don’t wait. Get tested.
Matt Beck
January 13, 2026 AT 23:14we’re all just meat sacks with faulty wiring, right?
OA? Your joints got tired of carrying your emotional baggage.
RA? Your immune system had a midlife crisis and decided to declare war on your knees.
gout? Your liver threw a party and invited uric acid.
we’re all just one bad burrito away from becoming a walking cautionary tale.
❤️
Molly McLane
January 15, 2026 AT 12:30I used to think arthritis was just creaky knees. Then I watched my mom go from hiking to needing a cane in 18 months.
She had RA. No one caught it early.
Now I ask every older relative: ‘Any morning stiffness? Swelling?’
It’s not paranoia. It’s love.
Tiffany Adjei - Opong
January 16, 2026 AT 16:27Wait-so if you have OA and RA at the same time, does that mean your body is just really bad at picking sides?
Also, I read somewhere that RA can be triggered by periodontal disease. So… are your gums the real enemy?
And why is no one talking about how insurance denies biologics unless you’ve tried 17 other drugs first?
And what if you’re allergic to methotrexate?
And why is ‘exercise’ always the answer? What if your joints are already shredded?
And why do all the ‘helpful’ articles ignore the mental toll?
Also, is it just me or does everyone on here act like this is a simple checklist?
It’s not.
It’s a mess.
And I’m tired.
Ryan Barr
January 17, 2026 AT 13:20Glucosamine is a placebo. Move on.
Lily Lilyy
January 18, 2026 AT 16:26To anyone reading this and feeling scared: you are not alone.
There are people who understand. There are treatments that work. There is hope.
Take one step today. Walk. Ask a question. Call your doctor.
You’ve got this.
And if today was hard? That’s okay. Tomorrow is a new day.
Keep going.
Rachel Wermager
January 20, 2026 AT 11:05Regarding the comment about OA and inflammation: while systemic inflammation isn’t the primary driver, local inflammatory mediators like IL-1β and MMPs are upregulated in OA synovium, particularly in obese individuals. This blurs the traditional dichotomy.
Additionally, the term ‘metabolic OA’ is gaining traction in the literature to describe OA associated with insulin resistance and adipokine dysregulation.
But this doesn’t negate the fundamental distinction from RA’s systemic autoimmunity.
Still, the boundaries are more porous than textbooks suggest.