Why Sleep Gets So Hard During Pregnancy
Many pregnant women think waking up tired is just part of the deal. But if you’re snoring loudly, gasping for air at night, or burning up with heartburn after dinner, it’s not normal fatigue-it’s your body signaling something deeper. Sleep apnea, acid reflux, and awkward positioning aren’t just annoyances; they’re medical issues that can affect both you and your baby.
By the third trimester, about 1 in 10 pregnant women develop obstructive sleep apnea (OSA). That number jumps to nearly 1 in 4 if you’re overweight. Your airway gets narrower because of swelling from hormones, extra fluid, and a growing belly that pushes up on your diaphragm. Your tongue and throat tissues relax more than usual, making it easier for your airway to collapse when you sleep. This isn’t just about poor sleep-it’s linked to higher risks of preeclampsia, gestational diabetes, and needing a C-section.
What Sleep Apnea Really Looks Like in Pregnancy
You might not realize you have sleep apnea because the symptoms overlap with regular pregnancy discomfort. Snoring? Common. Daytime fatigue? Expected. Morning headaches? Just stress, right? But if you’re waking up choking, your partner says you stop breathing for seconds at a time, or you’re exhausted even after 8 hours in bed, it’s time to get checked.
The gold standard test is a sleep study-either in a lab or at home with a portable monitor. These devices track your breathing, oxygen levels, and brain activity while you sleep. A diagnosis isn’t made just because you snore. Only about 12% of pregnant women who report snoring actually meet the clinical criteria for OSA. That’s why screening matters. The American College of Obstetricians and Gynecologists now recommends asking all pregnant women about sleep problems at their first visit using a simple questionnaire.
CPAP Therapy: The Most Effective Treatment
If you’re diagnosed with moderate to severe sleep apnea (an AHI of 15 or higher), CPAP is the first-line treatment. It’s a machine that blows gentle air through a mask to keep your airway open. Many women worry it’ll be uncomfortable, especially with pregnancy swelling, but modern devices are designed for this.
Today’s CPAP machines for pregnant women have features like auto-adjusting pressure, heated humidifiers set to 37°C to fight nasal dryness, and nasal pillows instead of full-face masks to avoid pressure on swollen cheeks. The ResMed AirSense 11 Pregnancy Mode, cleared by the FDA in 2022, automatically adapts to your changing breathing patterns as your pregnancy progresses.
Studies show starting CPAP between 24 and 28 weeks reduces the risk of preeclampsia by 30% and gestational hypertension by 35%. One woman in Philadelphia started using it at 26 weeks and saw her AHI drop from 18 to 6 in two weeks. Her blood pressure stabilized within days. That’s not luck-it’s science.
Adherence is the biggest hurdle. Only 62% of pregnant women stick with CPAP beyond four weeks. But when clinics add education and support-like a 30-minute fitting session and follow-ups at 3 and 7 days-adherence jumps to 82%. Don’t give up after a rough first night. It usually takes 7 to 14 days to adjust.
Positioning: The Simple Fix That Works
If your apnea is mild (AHI under 15), changing how you sleep can make a big difference. Sleeping on your back is the worst position-it lets your tongue and uterus press against your airway. Sleeping on your left side is the best. It improves blood flow to your baby and reduces pressure on your diaphragm.
Specialized pregnancy pillows help. The Boppy Noggin CPAP pillow, for example, is designed to hold you on your side while leaving space for your mask. One user wrote: “Finally a pillow that keeps me on my side without sliding-and my AHI dropped from 18 to 6 in 2 weeks.” Studies show left-side sleeping with support can reduce your apnea-hypopnea index by nearly 23%.
Don’t just prop yourself up with regular pillows. That can bend your neck and make apnea worse. Instead, use a wedge pillow under your upper body, elevating your head 7 to 8 inches. This helps with both breathing and reflux. A 2022 study found this position improved oxygen levels by over 3% compared to lying flat.
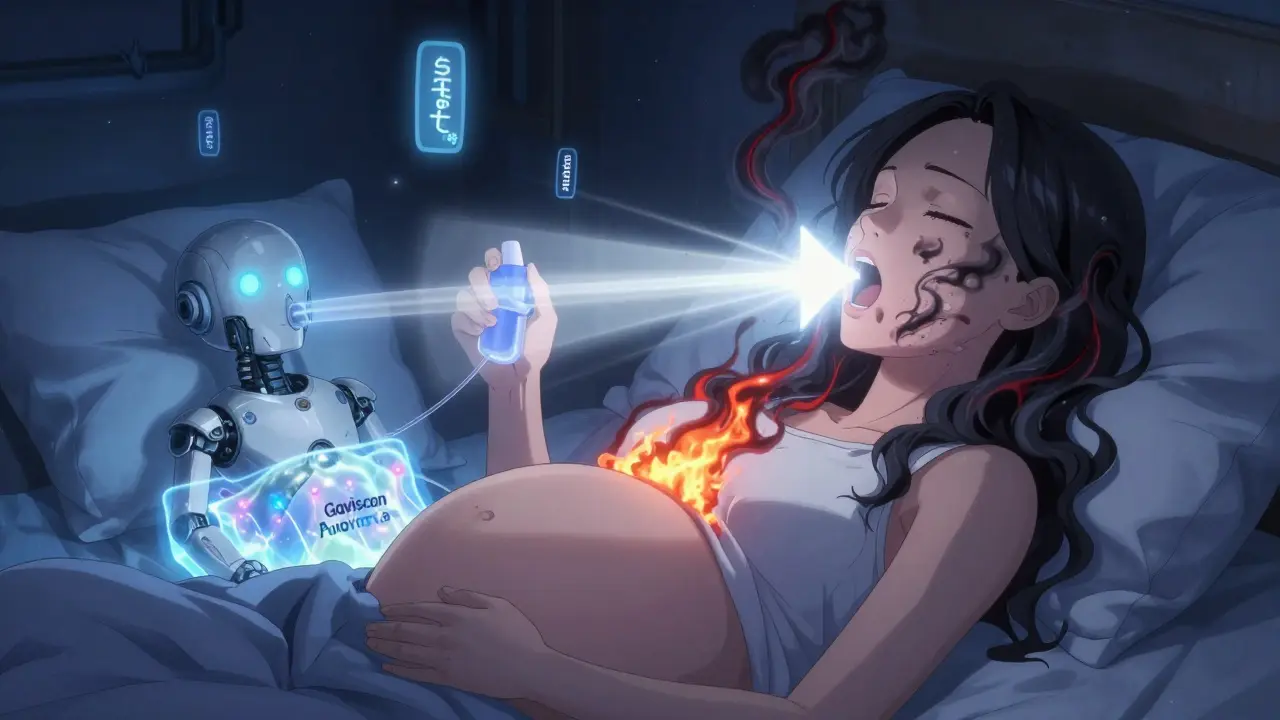
Taming Heartburn and Reflux at Night
Heartburn during pregnancy isn’t just spicy food-it’s hormones relaxing the valve between your stomach and esophagus, plus your growing baby pressing up on your stomach. Lying down makes it worse.
Here’s what actually works:
- Elevate the head of your bed 6 to 8 inches using blocks or a wedge-not just pillows. Pillows can push your neck forward and worsen apnea.
- Avoid eating within 3 hours of bedtime. Even a light snack can trigger reflux.
- Use Gaviscon Advance, an alginate-based antacid that forms a protective foam barrier in your stomach. It doesn’t get absorbed into your bloodstream, so it’s safe during pregnancy. A 500ml bottle costs around $15 and lasts weeks.
- Wear loose pajamas. Tight clothing adds pressure.
Many women think they just have to live with nighttime heartburn. But with the right strategy, you can sleep through the night without burning.
What Doesn’t Work (And Why)
Not every solution marketed for pregnant women is backed by evidence.
Mandibular advancement devices-mouthpieces that push your jaw forward-work well for non-pregnant people with mild apnea. But during pregnancy, your jaw and TMJ are already under stress from hormonal changes. There’s no safety data for these devices in pregnancy, and major guidelines advise against them.
Over-the-counter sleep aids? Avoid them. Even “natural” herbs like valerian or melatonin aren’t proven safe during pregnancy. And while some pillows claim to treat apnea, most haven’t been tested in clinical studies. Look for products that reference real data, like the Leachco Full Body Pillow Pro, which has been used in research settings.
And don’t wait until you’re miserable to act. The earlier you address sleep apnea, the better the outcomes. Each week of CPAP use before 28 weeks lowers your preeclampsia risk by nearly 5%.

What Happens After Baby Arrives
Many women assume their sleep apnea will disappear after delivery. For some, it does. But here’s the catch: 58% of women who developed sleep apnea during pregnancy go on to develop chronic high blood pressure within 10 years-even if their apnea seemed to vanish.
Some clinics, like Brown Health, recommend a follow-up sleep study at 12 weeks postpartum. Others, like the NIH, suggest watching for symptoms and testing only if problems return. Either way, don’t ignore persistent snoring, fatigue, or morning headaches after birth. Your body may still be recovering.
Real Stories, Real Results
On Reddit, a user named ‘ExpectingMom2023’ wrote: “CPAP saved my third trimester. My blood pressure stabilized within two weeks. But the mask leaked because my nose swelled.” She wasn’t alone. Forty-one percent of users quit CPAP because of discomfort. But with the right mask fit and humidifier settings, most can stick with it.
One mother in Sydney started CPAP at 25 weeks. Her husband said she stopped snoring completely. Her energy returned. She didn’t develop preeclampsia. “I thought I was just tired,” she said. “Turns out I was suffocating at night.”
These aren’t rare cases. They’re the norm for women who get screened and treated early.
What to Do Next
If you’re pregnant and struggling to sleep:
- Ask your OB-GYN about sleep apnea at your next visit. Don’t wait until you’re exhausted.
- Start sleeping on your left side with a wedge pillow under your upper body.
- Avoid late meals and use Gaviscon Advance if heartburn hits.
- If you snore loudly, wake up gasping, or feel constantly tired, ask for a sleep study.
- If CPAP is recommended, don’t fear it. Work with a sleep clinic that understands pregnancy-they’ll help you find the right mask and settings.
Good sleep isn’t a luxury during pregnancy. It’s medicine.
Can sleep apnea during pregnancy harm my baby?
Yes. Untreated sleep apnea is linked to a 42% higher risk of fetal growth restriction, preterm birth, and low birth weight. It also increases the chance of preeclampsia, which can force early delivery. CPAP therapy, especially when started before 28 weeks, significantly reduces these risks.
Is it safe to use CPAP while pregnant?
Yes. CPAP is not only safe-it’s recommended for pregnant women with moderate to severe sleep apnea. Modern devices have pregnancy-specific settings, softer masks, and heated humidifiers to handle swelling and dryness. Studies show it improves oxygen levels for both mother and baby.
What’s the best pillow for sleep apnea during pregnancy?
Look for a full-body pillow that supports side sleeping and has a cutout or groove for your CPAP mask. The Boppy Noggin CPAP pillow and Leachco Full Body Pillow Pro are two models used in clinical studies. Avoid regular pillows-they can tilt your neck and worsen apnea.
Can I use a mouthpiece instead of CPAP?
No. Mandibular advancement devices aren’t recommended during pregnancy. There’s no safety data, and hormonal changes can affect your jaw and TMJ. CPAP and positional therapy are the only proven, safe options.
When should I get tested for sleep apnea?
If you snore loudly, wake up gasping, or feel exhausted despite sleeping enough, ask for a sleep study. Screening is now recommended at your first prenatal visit. If you’re overweight or have high blood pressure, testing should happen by 28 weeks at the latest.
Will my sleep apnea go away after I have the baby?
It might, but not always. About half of women who develop sleep apnea during pregnancy still have it a year later. Even if symptoms disappear, you’re at higher risk for chronic high blood pressure in the future. Follow up with your doctor if you still feel tired or snore after delivery.
