Medication Tolerance Predictor
How long will your side effects last?
Tolerance happens at different rates for different side effects. Enter your medication type and side effects to see estimated adaptation times based on clinical research.
Select medication type and side effect to see prediction
How this works:
Tolerance develops differently for different side effects based on where they occur in the body. Brain-related side effects (nausea, dizziness) often fade within days or weeks as receptors adapt. Organ-specific side effects (constipation, sexual dysfunction) tend to persist because those tissues don't adapt as quickly. This tool uses real clinical data from studies to estimate how long you might experience specific side effects.
Ever start a new medication and feel awful for the first few days-nausea, dizziness, fatigue-only to have it all vanish after a week or two? Meanwhile, that constipation from your painkiller? Still there. Or the sexual side effect from your antidepressant? Doesn’t go away. It’s not just you. This isn’t bad luck or a glitch in your body. It’s tolerance-and it’s happening in ways most people never realize.
What Tolerance Really Means (And Why It’s Not Addiction)
Tolerance isn’t about becoming dependent. It’s not about craving the drug or needing it to feel normal. It’s your body adapting. When you take a medication over and over, your cells don’t just sit there and take it. They fight back. They change. They adjust. And that’s why some side effects fade while others don’t.
Think of it like turning up the volume on a speaker. At first, it’s loud. Too loud. But after a while, your ears adjust. The sound hasn’t changed-but your perception has. Your body does the same thing with drugs. It resets its sensitivity. This happens through three main pathways: how your body breaks down the drug, how your receptors respond, and how your cells rewire themselves.
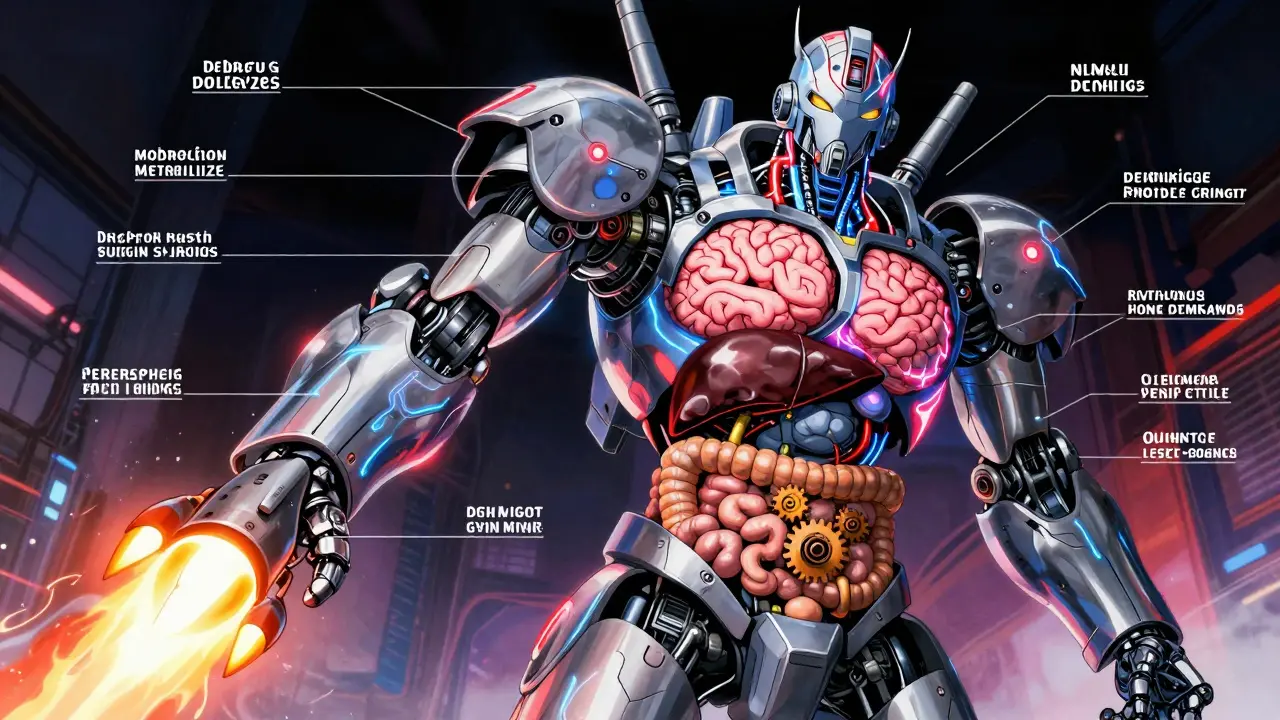
How Your Body Gets Used to the Drug (Pharmacokinetic Tolerance)
One big reason side effects fade is because your liver gets faster at cleaning the drug out. This is called pharmacokinetic tolerance. Your liver uses enzymes-mainly from the CYP450 family-to break down medications. When you take a drug regularly, your body says, “Hey, we’re seeing this a lot,” and starts making more of these enzymes.
For example, chronic alcohol use can boost CYP2E1 enzyme activity by up to 300%. That means alcohol leaves your system faster, so you feel less drunk over time. Same with barbiturates and some seizure meds-they trigger your liver to churn out more enzymes, reducing their own side effects like drowsiness.
But here’s the catch: this doesn’t help with every side effect. If a drug’s problem isn’t how long it stays in your body, but how it interacts with your brain or gut, then faster metabolism won’t fix it. That’s why nausea from opioids fades, but constipation doesn’t. The nausea is tied to brain receptors that adapt. The constipation? That’s the drug acting directly on your intestines-and your gut cells don’t adapt as quickly.
How Your Cells Turn Down the Volume (Pharmacodynamic Tolerance)
This is where things get really interesting. Pharmacodynamic tolerance is about your cells changing how they respond to the drug-not how fast it’s cleared, but how it’s received.
Your cells have receptors, like locks that drugs fit into. When you take a drug repeatedly, those locks can:
- Decrease in number (downregulation)
- Change shape so the drug doesn’t fit as well
- Stop sending signals even when the drug is bound
Take opioids. They bind to mu-opioid receptors in your brain. After a few doses, your brain reduces the number of these receptors by 20-50%. That’s why the euphoria and drowsiness fade. But those same receptors? They’re sparse in your gut. So your intestines keep getting the full force of the drug. Result? Constipation sticks around.
Same with benzodiazepines. They boost GABA, a calming neurotransmitter. After two weeks, your brain reduces GABA-A receptor sensitivity-so the sedation drops by 60-70%. But the anxiety relief? Still there at 85-90%. That’s because the brain circuits that control fear don’t downregulate as much. Your body is smart enough to keep what works and ditch what doesn’t.
Differential Tolerance: Why One Side Effect Vanishes and Another Doesn’t
This is the key idea: differential tolerance. Different parts of your body adapt at different speeds. It’s not one big switch. It’s a patchwork of changes across organs, receptors, and neural pathways.
Here’s what real patients report:
- 78% of opioid users on Reddit said nausea vanished within 3-7 days. Constipation? Still there for 92%.
- 65% of people on pregabalin (for nerve pain) said dizziness disappeared by day 14. No one said the tingling went away.
- 73% of SSRI users lost the initial nausea within 2-3 weeks. But 58% still had sexual side effects after six months.
- Patients on interferon for multiple sclerosis reported fatigue faded in 4-6 weeks-but injection site burns didn’t.
Why? Because nausea is controlled by brainstem receptors that adapt quickly. Constipation? Gut receptors don’t adapt. Dizziness? Inner ear and brain balance centers recalibrate. Sexual dysfunction? That’s tied to serotonin receptors in the spinal cord and pelvic nerves-areas that rarely reset.
This isn’t random. It’s biology. Your body prioritizes survival. It doesn’t care if you’re a little constipated. But if you’re too drowsy or nauseated, you might stop taking the drug. So it removes the barriers to adherence-while leaving the ones that don’t threaten your daily function.
What This Means for You (Practical Takeaways)
If you’re on a new medication and feel terrible at first, don’t panic. Give it time. For most side effects-nausea, dizziness, fatigue-you’ll likely feel better within 1-3 weeks. That’s normal.
But if something sticks around-like constipation, weight gain, or sexual issues-that doesn’t mean the drug isn’t working. It means your body hasn’t adapted to that specific effect. And that’s okay. You can manage it.
Here’s what to do:
- Don’t stop the medication just because you feel bad at first. Most side effects fade.
- Track what’s changing. Keep a simple log: “Day 1: dizzy. Day 7: dizzy gone. Still constipated.” This helps your doctor know what’s tolerance and what’s not.
- Ask about solutions. For constipation from opioids, laxatives are standard. For sexual side effects from SSRIs, switching to bupropion or adding low-dose sildenafil can help.
- Don’t assume worsening symptoms = more need for the drug. If your pain isn’t better after 3 weeks, it might not be tolerance-it might be disease progression.
When Tolerance Becomes a Problem
Tolerance isn’t always a good thing. Sometimes, your body gets so used to the drug that you need higher doses to get the same benefit. That’s when things get risky.
For opioids, this is especially dangerous. Tolerance to sedation can rise fast-within 24-72 hours. But tolerance to respiratory depression? That’s slower. So you might feel fine taking more, but your breathing could slow dangerously. That’s why doctors avoid increasing opioid doses without close monitoring.
Same with benzodiazepines. Tolerance to anxiety relief? That can happen after months. But if you increase the dose to compensate, you risk dependence, memory issues, and withdrawal seizures.
The trick is knowing what’s changing and why. A 2021 study found 25-30% of doctors misread worsening symptoms as tolerance when it was actually the disease getting worse. That’s why regular check-ins with your provider matter.
What’s New in Tolerance Research
Scientists are now designing drugs to fight tolerance itself. In 2023, the FDA approved a combo pill-naltrexone and bupropion-that blocks tolerance to opioid nausea without reducing pain relief. Early results show 45% fewer patients suffer long-term nausea.
Researchers are also testing polymer-coated pills that release opioids slowly, reducing receptor overstimulation. In trials, these pills cut tolerance development by 60% over 8 weeks.
And the future? Personalized medicine. Genetic tests can now identify if you’re a fast or slow metabolizer of certain drugs. About 7-10% of Caucasians have a gene variant (CYP2D6 poor metabolizer) that makes codeine useless. Others process it too fast, turning it into dangerous levels of morphine. Testing for this before prescribing can prevent side effects before they start.
Bottom Line: Your Body Is Adapting-Not Failing
Tolerance isn’t a flaw. It’s a feature. Your body is trying to keep you stable. It’s why you can take a beta-blocker for years without collapsing from fatigue. It’s why you don’t feel like you’re drunk on your anxiety med after a month.
But it’s also why some side effects never go away. And that’s not your fault. It’s biology. Understanding this helps you make smarter choices. Don’t give up on a medication because you felt sick at first. But don’t ignore side effects that stick around either. Talk to your doctor. Track what changes. And know this: your body isn’t broken. It’s just learning how to live with the drug.
Why do some side effects go away but others don’t?
Different parts of your body adapt at different speeds. Side effects tied to brain receptors (like nausea or dizziness) often fade because those receptors downregulate quickly. Side effects from direct organ action (like constipation from opioids or sexual dysfunction from SSRIs) stick around because those tissues don’t adjust as easily. This is called differential tolerance.
Does tolerance mean I’m addicted?
No. Tolerance means your body has adapted to the drug’s effects. Addiction involves compulsive use despite harm, cravings, and loss of control. You can have tolerance without addiction-like taking blood pressure meds for years and needing the same dose because your body adjusted, not because you’re dependent on the feeling.
How long until side effects like nausea or dizziness go away?
Most brain-related side effects-nausea, dizziness, fatigue-improve within 1 to 3 weeks. For SSRIs, nausea fades in 2-3 weeks for 73% of users. For opioids, vomiting stops by day 3-5 for most. If it hasn’t improved after 4 weeks, talk to your doctor.
Can I speed up tolerance to side effects?
No-and you shouldn’t try. Taking higher doses to “get used to it” can be dangerous. Tolerance develops naturally with consistent use. Pushing doses higher risks overdose, dependence, or worsening side effects. Stick to your prescribed dose and give your body time.
Why do I still feel tired on my antidepressant after 6 months?
Fatigue from antidepressants often fades within weeks. If it’s still there after 6 months, it’s likely not tolerance-it’s either the medication’s side effect persisting, or an underlying issue like low thyroid, poor sleep, or depression itself. Talk to your doctor about switching meds or adding a stimulant like modafinil or bupropion.
Are there medications designed to avoid tolerance?
Yes. New drugs are being developed to minimize tolerance. For example, polymer-coated opioids release slowly, reducing receptor overstimulation. Combination pills like naltrexone-bupropion block tolerance to nausea without affecting pain relief. Research into genetic testing is also helping match patients to drugs they’re less likely to develop tolerance to.
Kipper Pickens
January 27, 2026 AT 13:03Pharmacokinetic vs. pharmacodynamic tolerance is such a crucial distinction that gets glossed over in med school lectures. The liver enzyme upregulation mechanism-especially CYP450 isoforms-is underappreciated in clinical practice. What’s wild is how tissue-specific receptor downregulation creates this patchwork effect: brain adapts, gut doesn’t. That’s why opioid-induced constipation is basically a chronic condition for long-term users. No amount of laxatives fixes the root-it’s a receptor density issue, not motility. Fascinating how evolution optimized for adherence over comfort.
Aurelie L.
January 29, 2026 AT 10:28My SSRIs made me feel like a zombie for 3 weeks. Then boom-gone. But the libido? Dead. Forever.